Abstract
This paper, the second of a series of two, provides an introduction to treatment planning in implant dentistry for the general dental practitioner.
From Volume 43, Issue 6, July 2016 | Pages 522-528
This paper, the second of a series of two, provides an introduction to treatment planning in implant dentistry for the general dental practitioner.

Good treatment planning can only occur when based upon a thorough understanding of the principles of implant dentistry in general practice. These include:
The clinician should begin with the end result in view in terms of whole patient care, not limiting the treatment plan to the replacement of missing or failing teeth and their implant-supported restorations.
Patient expectations must be identified early in the consultation process and compared with a detailed case assessment to determine if they can be met. Much implant company marketing literature gives a very positive aesthetic outcome for implant-supported restorations, potentially setting the patients' expectations beyond what may be readily achievable. It is not the implant components that determine the aesthetic outcome but the time spent on case assessment in order to arrive at a correct diagnosis and treatment plan.2 The question ‘What can I do for you?’ should reveal their expectations. Implant restorations must provide both appropriate and achievable form and function. Providing function is a much more straightforward process than providing form.2,3
Answers to the question ‘What can I do for you?’ are crucial:
Answers 4 and 5 should be taken as warning signals.
Clear communication with the patient is essential from the outset. The use of educational models, clinical photographs and a diagnostic set-up are invaluable in conveying the appearance of the planned restoration.
Even when the required criteria to provide a long-term successful implant-supported restoration can be met, alternative treatments must be considered and discussed with the patient as part of the informed consent process. Priest suggests that the use of dental implants for the replacement of a single missing tooth helps preserve the adjacent teeth by sparing their use as abutments for fixed and removable partial dentures.4 He reports a 97.4% survival rate over a 10-year period but also describes complications such as loss of implant crowns, screw loosening, broken screws, cement washout, margin exposure and porcelain fracture. A review paper contrasts implant success against implant survival where the implant survival rate may be 100% vs 52% success in one study.5 The risks and benefits of each treatment option must be clearly described and discussed in terms that the patient can understand.
In cases where there is inadequate space in the vertical or horizontal planes to accommodate the implant restoration, orthodontic treatment may be indicated. On occasions, orthodontic extrusion prior to extraction has been suggested to improve the vertical position of the hard and soft tissue margins. The repositioned margins then allow for implant placement in a position that will provide a better aesthetic outcome.6
The following questions need to be asked:

Unlike natural teeth that benefit from the sensitive shock-absorbing features and mechanoreceptors of the periodontal ligament, osseointegrated implants are effectively ankylosed to the surrounding bone. Without the protective features of the periodontal ligament, implant restorations are more susceptible to occlusal overload that may lead to screw loosening, component fracture, porcelain fracture, bone loss and eventual implant loss. This susceptibility is brought into perspective when patients describe a solid wooden sensation on biting and chewing.7 Wolff's law8,9,10 basically states that bone growth and remodelling throughout life shows adaptation to the mechanical environment. Restorations should be planned so that they do not cause occlusal intolerance that exceeds the adaptive capacity of the bone11 to avoid bone loss.12 The bone/implant interface should be loaded within the physiological tolerance of the patient's bone, for example by using a reduced occlusal table and low cusp angles. Extreme care is required to protect the bone implant interface.
If the presenting alveolar foundation will not allow a successful implant restorative outcome then that foundation may have to be augmented with soft tissue, hard tissue or both. If this is not feasible then an alternative treatment plan must be followed. What the clinician should ask is ‘What are the benefits to the patient?’13 and are they achievable without complications? It is essential that the GDP must be competent to carry out the procedure.
Retzepi and Donos14 reviewed the biological principle and therapeutic applications of guided bone regeneration (GBR) for the following:
They concluded that GBR can predictably lead to the regeneration of bone in each of these scenarios. An occlusive membrane is used to avoid the ingress of soft tissue into the bone graft material and space must be maintained for augmentation in the vertical or horizontal dimension or both. Socket preservation with particulate graft material alone (ie without the use of an occlusive membrane) may actually interfere with the normal bone healing process. However, it is important to point out that complications with GBR techniques are common.13,14
There may be a need to consider soft tissue augmentation before, during or after implant placement. The approach and material used will be determined by the desired objective. A systematic review investigated the efficacy of soft tissue augmentation around dental implants and in partially edentulous areas.15 It concluded that the sub-epithelial connective tissue graft is the treatment of choice for soft tissue bulking in both the implant and partially edentulous site. The authors highlighted the lack of studies for gain in keratinized mucosa and also that many of the studies were company sponsored, introducing the potential for bias.
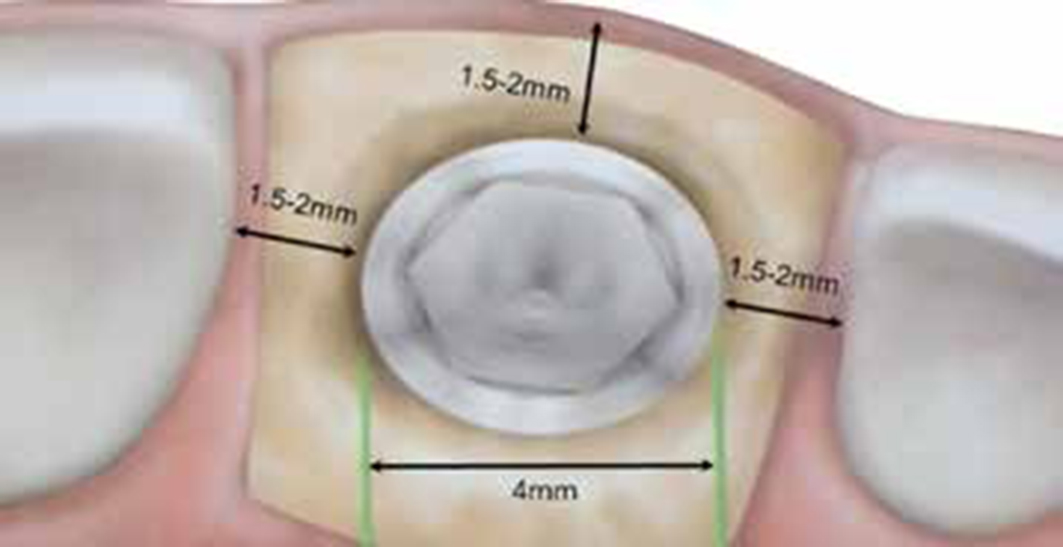
Useful information can be obtained from the existing restoration, and in the partially dentate situation measuring the space available for the implant-supported restoration. The number of implants required will partly be determined by the type of restoration, fixed or removable, the location of the restoration and the space available. The inter-implant distance should be at least 3 mm if crestal bone and the inter-implant papilla are to be maintained between the implants16 (Figure 2). A recent study showed that the use of a platform-switched implant design (that is the diameter of the abutment is less than the diameter of the implant at the level of the implant abutment interface) allows for the inter-implant distance to be less than 3 mm while still maintaining the inter-implant crestal bone level.17 The platform-switched implant design has been shown to help maintain crestal bone levels and support the overlying soft tissue contour18,19
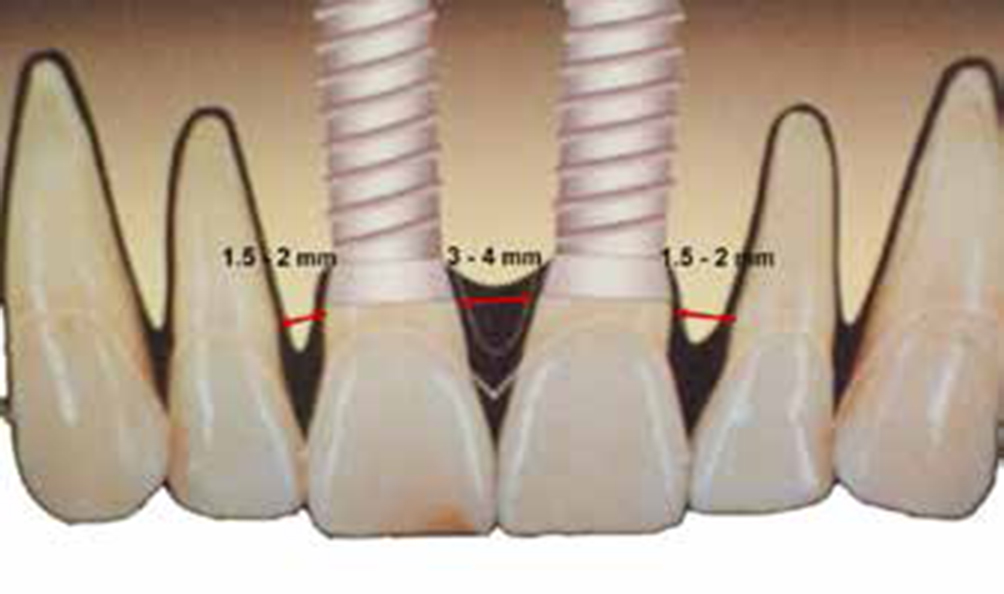
A dilemma arises when the interproximal space in the partially dentate situation does not readily allow for these spacing criteria to be applied. The practitioner must then consider the use of ancillary treatment, eg the creation of space by orthodontic treatment, the use of larger or smaller diameter implants bearing in mind the loading of the implant(s), the emergence profile of the restoration, distance to adjacent structures (Figure 3) and the option to use a cantilever design restoration.
This is a most important component of treatment planning, since a poorly designed or ill-fitting provisional restoration has the potential to undo the work of the most skilful clinician, whereas a well-designed and well-fitting provisional restoration has the potential to sculpt the tissues and contribute to a positive aesthetic outcome. It is also of paramount importance that, for both the provisional and definitive restoration, the implant clinician works hand in hand with a laboratory/dental technician knowledgeable, skilled and experienced in implant dentistry.
The provisional restoration may be fixed or removable or, in some cases, not required, for example if the restoration is outside of the ‘aesthetic zone’. It may be tooth-supported (eg adhesive bridge or a modified Essix appliance), soft tissue-supported or supported with temporary implants. Where the patient has an existing partial denture, this may serve as a provisional restoration, although care needs to be taken to ensure that the denture does not apply pressure to the underlying implant and/or graft material.
When starting with the end point in view, the diagnostic set-up may be used for the provisional restoration and will help determine the ideal position of the implant(s) from the restorative perspective rather than simply placing the implant(s) in the region of the greatest volume of bone. In general terms the ‘Spoon’ denture design should be avoided as it has the potential to apply damaging pressure to the underlying tissue/implant. When the final restoration is to be of a fixed design, buccal/labial flanges on removable partial denture prostheses should also be avoided as these can lead to wound breakdown after implant placement and also give the patient a false impression of lip support when compared with the final restoration.
This may be fixed or removable, and may comprise single or multiple units, in which case the question arises should the units be linked or separate. The restoration may be screw-retained or cement-retained. The screw-retained restoration favours retrievability but may compromise aesthetics. The cement-retained restoration can favour aesthetics but may compromise long-term survival of the restoration due to lack of detection and removal of excess cement when the restoration is fitted. Failure to remove excess cement has been implicated as a major cause of periimplantitis.20,21 The deeper the position of the crown margin, the greater is the likelihood of excess cement being undetected and only when the crown margin is supragingival can all excess cement be assured of removal, which paradoxically may compromise aesthetics.22
The implant-supported cantilever restoration remains a controversial issue. Misch recommends that, if a cantilever design is to be used, the cantilever should be extended mesially and cantilevers based upon two implants should be avoided.23 Others conclude that the presence of a cantilever has no impact on marginal bone loss, with the exception of the posterior mandible.24 However, the presence of a cantilever is associated with significantly more technical problems at the implant level.
The connection of implants to teeth also remains a controversial issue. It is generally accepted that this should be avoided though, if required, the implant should be linked to a tooth distal to it owing to the inherent movement of teeth within their sockets; the more posterior the tooth the less is its movement.23 However, some studies suggest that linking natural teeth to implants can be successful with careful patient selection and choice of materials.25
The majority of patients seeking implant treatment consider implants as natural teeth and want to have those teeth as quickly as possible. The practitioner has the option of following a number of protocols ranging from immediate substitution, whereby a tooth or teeth are extracted and immediately replaced with a functional, albeit temporary restoration, to delayed implant placement with the restoration some 3–6 months after implant placement, in other words a single or two-stage approach. In a two-stage approach the implant is placed and primary closure achieved. After a period to allow for osseointegration, second stage surgery is required to expose the implant (Figure 4). This differs from single stage surgery where a healing collar/healing abutment is placed at the time of surgery (Figure 5). Should augmentation be required prior to implant placement, this can significantly delay the provision of the definitive restoration. It is essential that the practitioner clearly conveys to the patient the treatment timescale.


Basic aftercare instruction must include maintenance of oral hygiene around the implant-supported restoration and the mouth in general. It should be both written and verbal and adequately demonstrated to the patient. The issue of peri-implantitis has been highlighted as an ‘important and growing health problem’.26 In the same debate it was stated that ‘as patients we would expect to receive sound advice from appropriately trained dentists performing implant procedures’. In summary, the debate highlights the need for appropriate patient information and aftercare. This situation was further substantiated in a paper published in the British Dental Journal in July 201527 that concluded that current education in the UK does not instil confidence in GDPs to provide and maintain dental implants. As periodontal and occlusal status can change with time, it is essential that an ongoing maintenance regimen is an integral component of treatment planning, informed consent and patient compliance.
This paper considers important aspects of treatment planning in implant dentistry. Each is worthy of much more deliberation well beyond the scope of the paper. The GDP must seek appropriate education and training in implant dentistry in line with GDC/FGDP guidelines before undertaking any implant treatment.