Abstract
This article is an introduction to single implant abutments and aims to provide basic information about abutments which are essential for all dental personnel who are involved in dental implantology.
From Volume 40, Issue 1, January 2013 | Pages 7-17
This article is an introduction to single implant abutments and aims to provide basic information about abutments which are essential for all dental personnel who are involved in dental implantology.

Dental implants are widely used and have proved to be a valid treatment with a high success rate.1 This high rate is due to the ability of the implanted material to integrate with the surrounding bone.2 Dental implants are used in restoring completely edentulous jaws as well as in replacing single and multiple missing teeth. The dental implant which is used to replace a single missing tooth usually consists of the implant body and the abutment to which the restoration will be attached. Several implant systems and abutment types are available from different manufacturers and familiarity with all of these types may be difficult.
There is a variety of dental implant systems available in the market worldwide, but only a few brands with an ADA seal of approval. Among these are Straumann, Nobel Biocare, Astra Tech, BioHorizon, Intralock, Biomet 3i, Zimmer and Bicon. Although they differ in patented technology, materials, and historical case success rates, they are all based on the same basic concepts. Also, there are different types of abutments available for implant systems which will be discussed at the end of this article.
Implant systems can be classified as a one- or two-piece implant system. In the one-piece (one-stage, non-submerged) implant system, the interface is usually placed supra-gingivally. In the two-piece (two-stage, submerged) system, the interface between the implant and the abutment is usually placed at/or below the crest of the bone. The implant-abutment connection is associated with a gap which is known as micro-gap. Bacteria were found to invade the micro-gap and create microbial colonization.3 When this microbial colony is close to the peri-implant tissues, bacteria induced inflammatory responses and crestal bone loss are found irrespective of the implant placement technique used. However, in one study,4 the crestal bone resorption around two-piece titanium implants was found to be significantly influenced by possible movements betweend the implants and abutments, but not by the size of the micro-gap, as this bone loss was found to occur even when the micro-gap was less than 10 microns.3
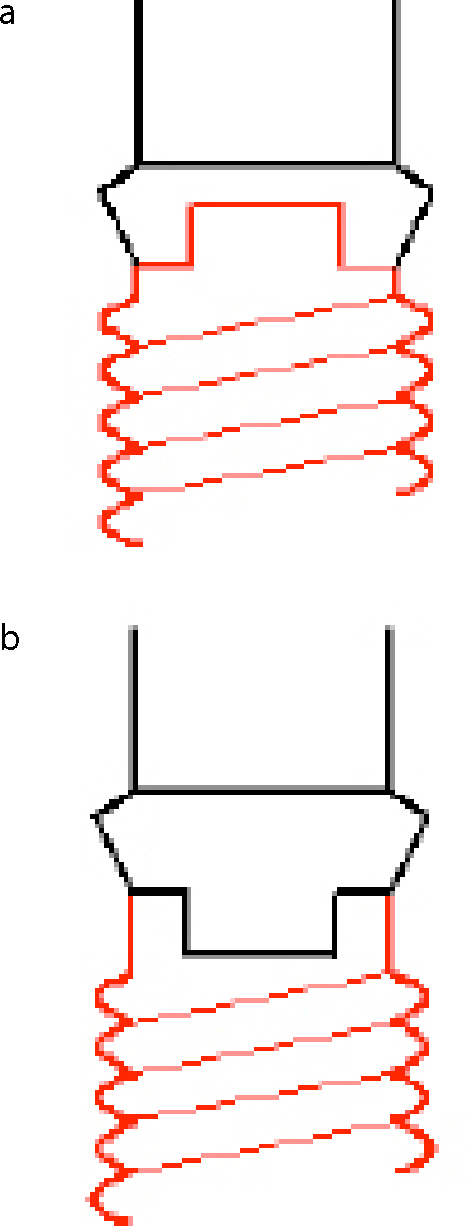
The implant-abutment connection may be classified as a butt- or a slip-joint. While the butt-joint is characterized by having two parallel flat contacting surfaces, the slip-joint has internal ‘cone-in-cone’ design. The latter design has more mechanical advantages than the butt-joint.5 The implant-abutment connections can be further categorized as either external, when it protrudes above the implant platform, or internal, when it is projected down in the access hole inside the implant body (Figure 1).
The external hex design was the first to be used in the manufacturing of dental implants. It was originally 0.7mm in height and was used to help screw the implant fixture into the prepared osteotomy. It was not used as an anti-rotational device because the rotation of the implant-supported restoration was not an issue. However, when the dental implants began to be used in replacing a single missing tooth, the external hex with some improved quality was used to prevent rotation of the abutment under loading. The external hex connection is still in use as it is suitable for the two-piece implant placement method, has an anti-rotation mechanism and is compatible with different implant systems. The external hex also helps the laboratory technician achieve the best possible emergence profile, as the porcelain can be brought closer to the implant-abutment interface. However, it is not without disadvantages, such as low resistance for rotational and lateral movements owing to its high centre of rotation. Furthermore, difficulty in seating the abutments in a deep gingival sulcus, increased screw loosening and component fractures are problems to be considered when the external hex connectors are used.
To improve the outcome of implant therapy and to overcome the complications and difficulties associated with the use of external hex connectors, a range of other connector types, such as internal connectors with a hexgonal or octagonal geometry and the ‘Morse’ taper, have been developed.
The internal hex connector is widely used. It is a stable connection with a high resistance to lateral forces because of the lower centre of rotation and is also suitable for a one-stage implant placement technique. It is also characterized by a good distribution of imposed force. However, weakening of the lateral wall of the implant at the connecting part, and compensation for mismatching in the angle between implant fixtures, may cause some problems.
The introduction of the internal hex connection concept was followed by the use of different geometries of connecting parts that engage the mating surfaces. For instance, the octagonal connector in which the number of sides are eight and the angle between each two adjacent sides is 45 degrees as compared with six sides and a 60-degree for the hexagonal one. A double hex connector is another internal connector type that consists of a hex and a 12-point double hex. The hex assists at delivering the implant into the osteotomy and provides an anti-rotational effect. The 12-point double hex allows 30-degree rotational flexibility for placement of pre-angled abutments.
Another design known as ‘Morse’ taper was also used. In the ‘Morse’ taper design a conical abutment post is engaged with the corresponding smooth non-threaded slot within the coronal part of the matching implant. It is assumed that the conical connections have the potential of better sealing the micro-gap between the abutments and the implants.
Another design on the market incorporates both an internal conical part (‘Morse’ taper) and a hex. It has been claimed that the conical part will provide a seal and stable relationship between the implant and the abutment, while the hexagonal part will act as an anti-rotational and indexing device.
A tapered internal connection with an intimate contact (friction-fit) between the abutment surface and the implant may generate an effective ‘cold weld’ between the two mating surfaces. As the occlusal force is distributed deeper within the implant, the abutment screw will be protected from the excessive loading. Elimination of rotational and tipping micro-movements reduces the possibility of screw loosening problems. Furthermore, the friction-fit connection between the abutment and the implant provides a good seal for the internal hollow of the implant from possible marginal leakage and bacterial contamination.
There is a general consensus that deep internal connections, in which the screw takes little or no load and provides intimate contact between mating surfaces, will result in good resistance to micro-movement. This movement may be associated with crestal bone loss, as has been mentioned earlier.4
In order to simplify the technique of placement of the abutments, an audible and tactile ‘click’ feature was incorporated in the internal connection. Thus, the clinician will be able to tell when the abutment is in its intended position on the implant and the need for a radiograph following placement may be reduced. The internal connection when it is long enough may provide lateral stability for the restorative component from off-axis occlusal forces.
There are currently about 20 different implant-abutment connection designs on the market.
These features are detailed in Table 1. A schematic representation of the external and the internal connections is seen in Figure 1.
| 1. According to the mating surfaces |
| 2. According to the nature of fit between the implant and the abutment |
| 3. According to the shape (geometry) |
It is generally acknowledged that the soft tissue that surrounds the teeth and the implants has several similar features.4 Therefore, the peri-implant soft tissue consists of two components:
Collagen fibres arise from the crest of alveolar bone and periostium and are oriented parallel to the implant surface towards the oral epithelium.7 Circular and horizontal fibres, which run perpendicular to the implant surface, were also found in the area.6 However, the oral gingival epithelium is keratinized.
The position of the junctional epithelium and connective tissue is highly affected by the material from which the implant abutment is made. While commercially pure titanium promotes healing which results in integration between the abutment surface and the surrounding soft tissue, gold alloy, for instance, does not encourage such healing and the soft tissue attachment is present, but on the implant-titanium surface and, consequently, this leads to the crestal bone resorption.
It is not unreasonable to assume that the peri-implant soft tissue makes a protective seal between the oral environment and the peri-implant bone and plays a vital role in the success of the implants.6
In order to achieve optimum aesthetic results, papilla and marginal gingiva must be healthy and supported by bone. The level of peri-implant soft tissue is dependent on the level of bone crest. Following the implant placement, recession of the soft tissue margin was observed and was attributed to bone and soft tissue remodelling, therefore the connective tissue and the junctional epithelium tends to migrate apically beyond the implant-abutment interface.
It has been suggested that the abutment design and the implant-abutment connection play a critical role in improving soft tissue outcomes.8 The bone crest was always found to be about 2mm below this micro-gap at the implant-bone connection.8 This level appears to be persistent irrespective of where the implant–abutment connection is situated relative to the original level of the bone crest.
Dental implant systems are characterized by their smooth trans-mucosal part of the abutments. The profile of this part of the abutment may be described as divergent, concave or straight. However, the mucosa was found not to be attached but simply adherent to smooth surfaces. To maintain the peri-implant tissue at its optimal level, rough trans-mucosal surfaces have been suggested.9 This was because the collagen fibres were found to penetrate the pores of the oxide surface that may enhance mucosal adhesion. Furthermore, it has also been recommended that the trans-mucosal part of the abutment should be concave for better and more predictable soft tissue stability, as more circular oriented fibres were found around the concave abutments than around the abutments with a straight or divergent profile. This may help in maintaining the tissue in its optimum position. It has been speculated that divergent walls of the conventional abutments may compress and make the peri-implant soft tissues thinner and susceptible to recession.9
This concept was based on clinical observations from the submerged implant methods which indicated that, when wide-diameter implants were connected with narrow-diameter abutments, the radiographic follow-up demonstrated a smaller vertical crestal bone loss around these implants when compared with abutments of the same diameter.10 Consequently, the platform-switching concept has been proposed in an attempt to overcome the occurrence of unfavourable vertical and horizontal crestal bone loss (saucerization) by preventing formation of a zone of connective tissue infiltrated with chronic inflammatory cells at the micro-gap region of the two-piece implant system. According to the platform-switching concept, the micro-gap is moved inward away from the bone, which allows the bone tissue to maintain a higher level of interface with the implant surface. The platform-switching approach also has the proposed biomechanical benefit of shifting the stress concentration away from the cervical bone-implant interface, which may be a co-factor in reducing the crestal bone resorption.11 However, several studies on a selected range of different types of implant systems show that the platform-switching method reduces, but does not completely inhibit, the crestal bone loss.10 Furthermore, other studies indicate that the major drawback of this technique is increasing stress in the abutment or abutment screw.11
The connection between the mating surfaces of the implant components which are tightened together by a screw is known as the screw joint.12 In general, there are one or two screw joints, depending on whether cement- or screw-retained restorations are used. If a cement-retained restoration is used, the screw joint is found between the implant body and the abutment. On the other hand, in a screw-retained restoration, the joint may be between the implant and the restoration or, if two joints, one between the implant and the abutment and the other joint between the abutment and the restoration. There are two different forces acting on any screw joint when the screw is tightened: one tries to keep the joint together and is known as the clamping force and the other tries to disengage it and is referred to as the separating force.12,13 As a tightening torque is applied to the screw joint, a tension (pre-load) is generated in the screw. Consequently, the screw shank and threads are placed in tension and an elastic recovery is generated. This elastic recovery creates the clamping force between the mating surfaces.12,13 The pre-load is effective if it is less than the elastic limit of the screw material as no permanent plastic deformation would occur.14 The generated pre-load depends on several factors, such as the screw material, the design of the screw head and the torque value.12
On the surfaces of new screws, microscopic surface roughness and irregularities (asperities) are usually present. The tightening of the screw causes friction between the mating surfaces and consequently the asperities are flattened and worn down. Therefore, more energy is dissipated in the smoothing of these asperities than in elongation of the involved screw. Subsequently, the mating surfaces are brought closer and the generated pre-load is reduced.13
In general, when the occlusal force is applied, fulcrum points are created between the two mating surfaces. If the mating surfaces are precisely fitted and the occlusal force vector is parallel to the axis of the screw at the screw joint, the fulcrum points are circumferentially arranged and the force is unlikely to stress the screw and it does not become loose.15 However, when the mating surfaces do not properly fit each other and spaces exist between the two mating surfaces, the forces which are applied off the fulcrum points try to separate the screw joint and, as a result, the screw will eventually become loose or even break.
It may be concluded that, in order to hold the implant components together and to keep the screw tight, a maximum clamping force and a minimal separating force are required. When the separating forces overcome the clamping forces, or when these forces are greater than the ability of the screw to keep the components together, the screw will become loose or break.12,15
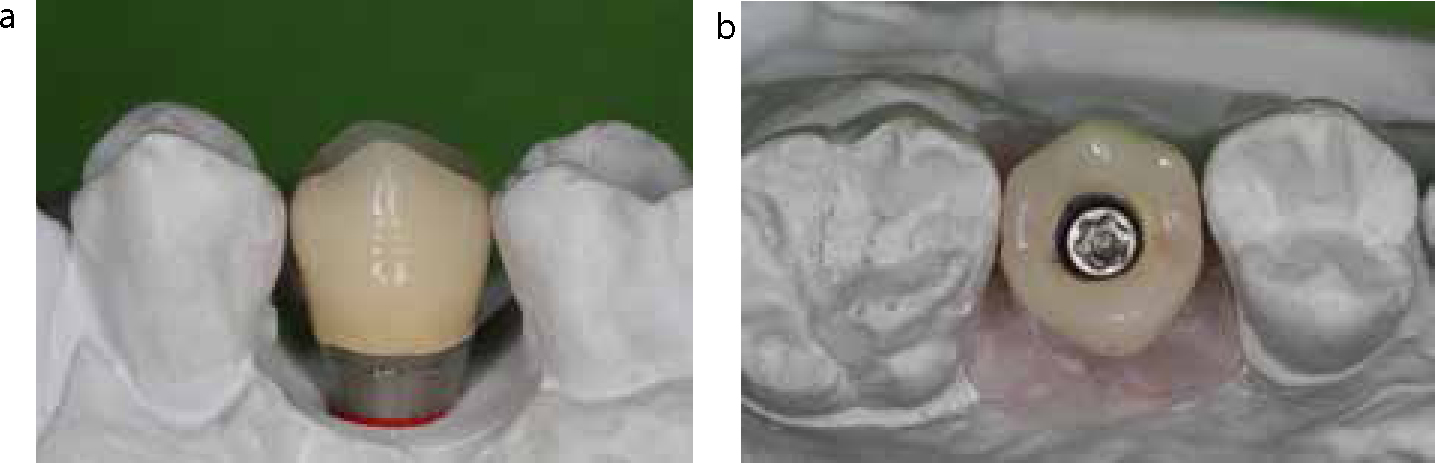
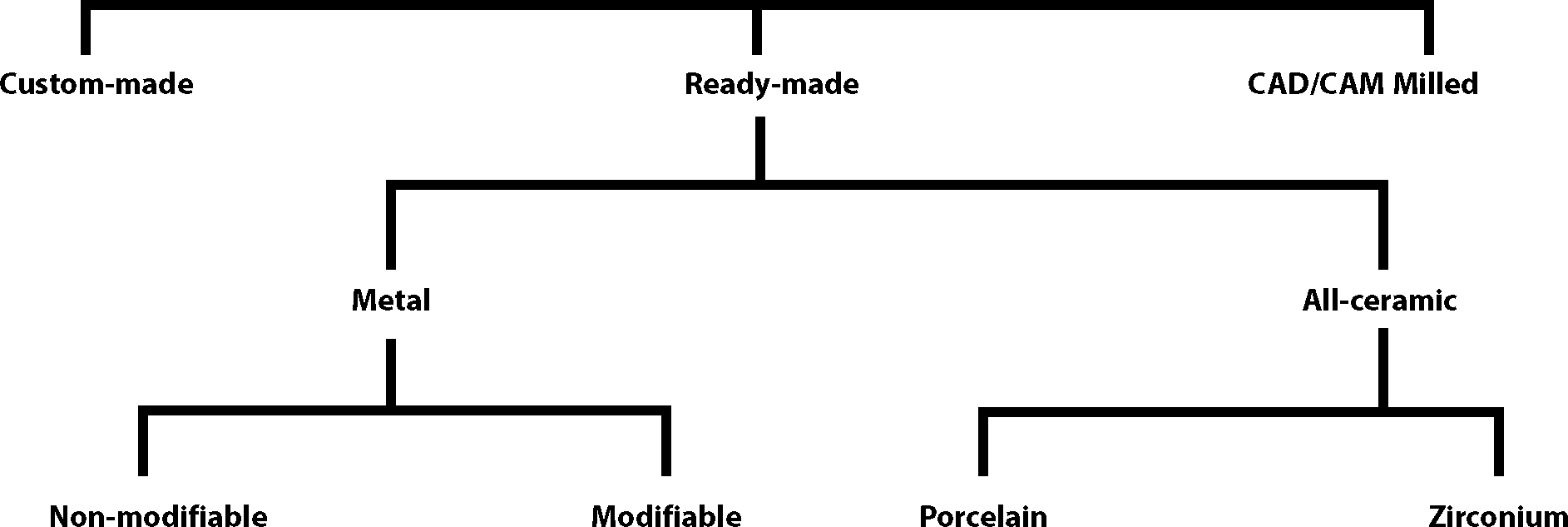
Implant-retained restorations may be divided into two types according to the method by which they are attached to the implant: screw- and cement-retained implant restorations (Figure 2). In the screw-retained implant restorations, the restoration is attached to the implant directly or to the abutment, while in the cement-retained ones, a cementing medium is used to retain the restoration on the abutment. Table 2 shows the advantages and disadvantages of cement- and screw-retained techniques.16 Generally, implant abutments may be further categorized as follows.
| Screw-type | Cement-type | |
|---|---|---|
| Retrievability | Restorations can be removed/replaced without damage or the need for a new restoration. | It is possible if weak cements were used, ie soft provisional cement, otherwise restorations have to be cut in order to remove them. |
| Inter-occlusal space/retention | Can also be used when the inter-occlusal space is limited, ie less than 4 mm. | Minimum inter-occlusal space with minimum converges are needed to achieve an optimal retention. |
| Limitation of mouth opening | The mouth opening should be enough for the use of different tools required for screwing and torquing the screws. | A restricted mouth opening is less problematic than with the use of the screw-retained restorations. |
| Occlusal loading | Unlikely to reduce the occlusal load on the restoration and the implant body. | The use of soft provisional cement may reduce the occlusal load on the restoration and the implant body. |
| Peri-implant inflammation | The adaptation between the restoration and the underlying implant is significantly better than that in the case of cement-retained counterpart. | The difficulty of removing the cement and the inferiority of margin adaptation between the restoration and the abutment, when this margin is placed subgingivally can cause peri-implant soft tissue inflammation. |
| Aesthetics and occlusion | The implant needs to be placed in its optimal angulation in the anterior zone. |
Even if the implant angulation is not optimal the restoration could still have good aesthetics. |
| Cost | The cost in terms of laboratory time and materials is much more than that for the cement-retained restorations. | The materials and techniques used for the fabrication of the conventional restorations can be used in this situation. |
This class consists of ready-made metal abutments which can be used without modification so that an abutment, which is suitable for the specific clinical condition, is selected and attached to the implant body. By using this type of abutment, the impression technique is simplified as the impression of the implant platform may not be needed because the impression of the abutment itself is sufficient. A manufacturer-made impression coping is used in making the abutment impression. These abutments can be temporized using the clinical resources available, as in the conventional crown and bridge procedures. This type of abutment can be used when the implant position imitates the position of the tooth being replaced, so the abutment can be placed in the correct position without modification. However, this abutment type suffers from a drawback because it is purely metal, greying the peri-implant soft tissue and showing through the cervical part of the abutment, which is unfavourable when aesthetics are the main concern. Metal greying was suggested earlier in the literature as a drawback for these abutments. This greying in the peri-implant mucosa is a result of light reflection as perceived by the human eye. However, when zirconium or titanium abutments were used, the difference in light reflection was not noticeable when the thickness of the mucosa was greater than 2 mm.17 Thus, the thickness of the peri-implant mucosa seems to play an important role in the aesthetic outcome of the implant-retained restoration.
The colour of the marginal peri-implant soft tissue was found to be affected by the material from which the implant-retained restoration was made. For instance, a significantly better soft tissue colour match with the marginal gingiva of neighbouring teeth could be achieved with all-ceramic restorations than with the porcelain fused to metal restorations.17
An example of the ready-made non-modifiable metal abutments is Snappy Abutment® (Nobel Biocare, AB, Göteborg, Sweden) with a relatively short profile which favours its use when the restorative (occluso-gingival) space is limited.
These types of abutments are ready-made metal abutments but these can be adjusted and shaped to meet a specific clinical situation. They have several metal collar heights to choose from, or alternatively the facial margin could be cut close to the implant platform allowing the margin of the final restoration to be located close to the implant-abutment interface and/or below the gingival margin. These abutments can be prepared and modified intra-orally and/or extra-orally on a master cast.12,18 Since they are made of metal, they hold the same disadvantages as the non-modifiable ones. Furthermore, reshaping and adjusting the abutment may be time consuming. They are also not suitable for many clinical situations, such as when the implant is severely angulated and a major alteration is required. Nevertheless, they are relatively easy to use.18
Easy Abutment® (Nobel Biocare) is an example of ready-made modifiable metal abutments.
To minimize the grey colour of titanium, other metal alloys are used or titanium may be coated with a more pleasant colour. GingiHue Posts® (Biomet 3i, Palm Beach Gardens, FL, USA) are titanium abutments that are coated with gold-nitride (yellow colour) which gives the abutment a natural hue through the peri-implant soft tissue. Gold alloy machined UCLA abutment is another example of ready-made modifiable abutments.
These abutments consist of a plastic/wax pattern with/without a metal machined interface ring. The metal-machined interface ensures a precise fit with the implant platform. The implant level impression is taken in the usual way. In the laboratory, the abutment plastic pattern is attached to the implant analogue on a working cast.18 The plastic pattern is cut to the required form, shape and angle then cast in metal alloy in a similar fashion to the conventional wax-lost technique. The restoration that fits the abutment is then fabricated (Figure 3).
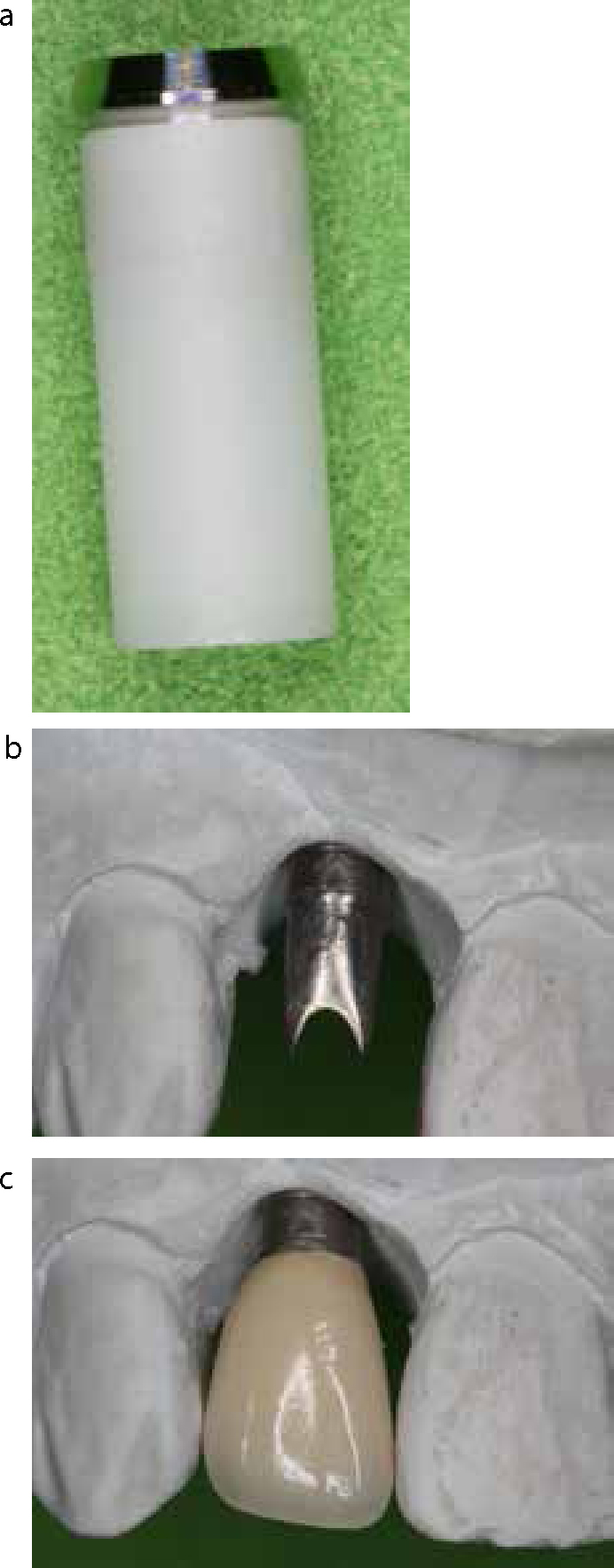
Custom-made abutments suit almost any clinical situation, regardless of whether the implant body is in the correct position or not, because it can be reduced as well as added to.18 These abutments can also be employed when the inter-occlusal space is limited. By using these types of abutments, the porcelain can be extended sub-gingivally and backed directly on the abutment, as in the case of screw-retained restorations.
UCLA plastic patterns are an example of these types of abutments (Figure 3). They are either made of a complete plastic pattern or plastic pattern with a machined interface. UCLA plastic patterns are either with an anti-rotational attachment (hexed) or without one (non-hexed). The former one is used for a single-tooth restoration and the non-hexed is used for implant-retained fixed prostheses. Nevertheless, it has been shown that the custom-made UCLA abutments provide an inferior fitting to the implant platform compared to ready-made modifiable UCLA abutments.19
Replacement of missing teeth in highly aesthetic zones using dental implants is a demanding task. In some clinical situations, when the aesthetic is of paramount importance, all-ceramic abutments are considered as an ideal solution.20 Improved aesthetic outcomes can be predicted when an all-ceramic abutment and crown are combined.21
In general, all-ceramic abutments are available in ready-made forms and are made of sintered aluminium oxide ceramic or yttria stabilized zirconia polycrestal ceramics.22 These abutments are modified and prepared in the patient's mouth or in the laboratory (Figure 4). Alumina abutments are easy to prepare when compared with the zirconia type. However, alumina has a low fracture resistance and appears opaque radiographically, while zirconia abutments are more fracture resistant and are whiter than alumina.22
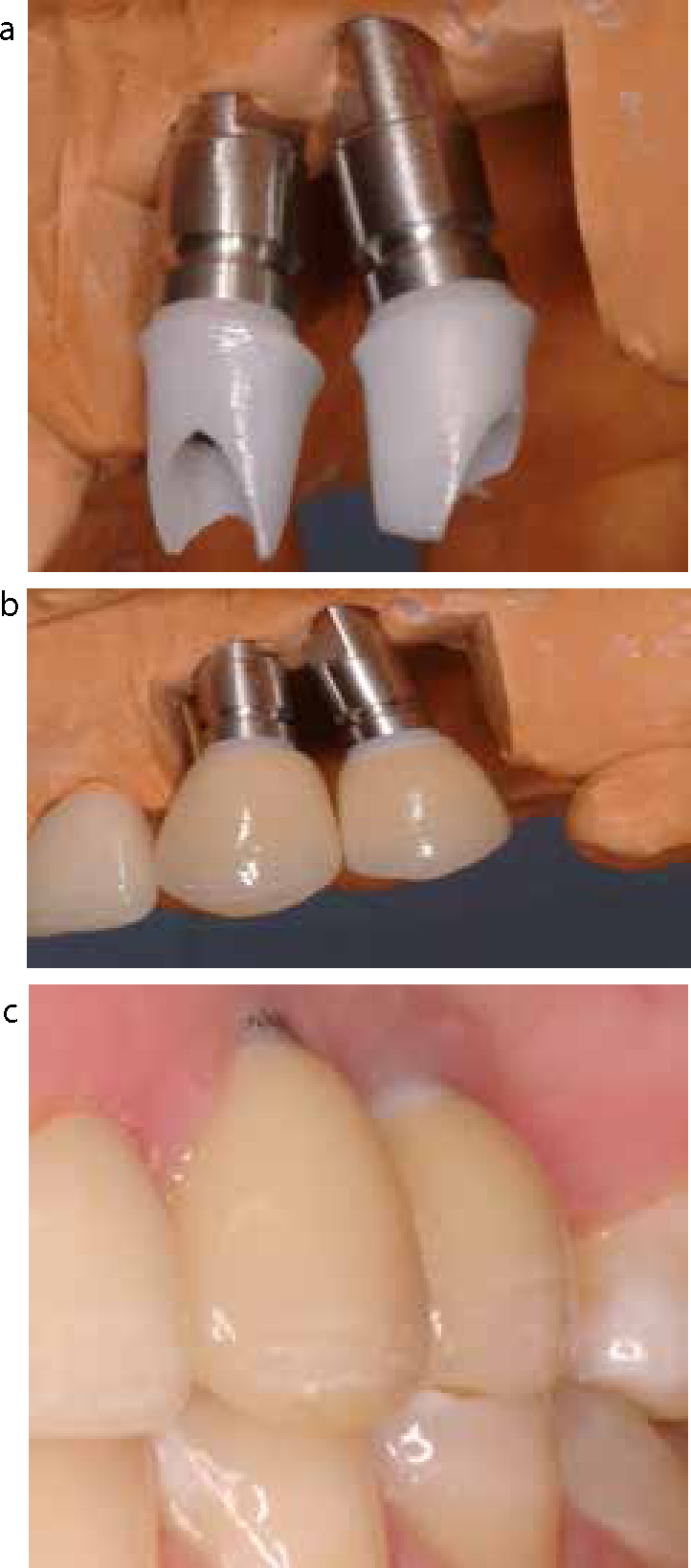
Use of all-ceramic abutments requires an implant platform impression and a working cast. The abutment is then modified in the laboratory and fixed to the implant by the recommended abutment screw. Subsequently, the final restoration is fabricated and cemented. However, all-ceramic abutments are recommended for use in single tooth crown restorations.22
Several advantages can be achieved when all-ceramic abutments are used. For instance, when the implant body is extended into the gingival sulcus, there will be no significant negative effect or discoloration of the gingival tissue. All-ceramic abutments may also be indicated in cases of thin biotype gingivae, so the bluish colour of the gingival tissue, which is reported to occur with the metal abutments, is avoided.21 All-ceramic abutments are also recommended when the planned final restoration will be an all porcelain one (Figure 4).
Zirconia and alumina Procera Abutment® (Nobel Biocare) and ZiReal postsTM (Biomet 3i) are examples of all-ceramic abutments.
Computer-aided design and computer-aided manufacturing (CAD/CAM) technology has been in use in dentistry for more than two decades.23 Originally, the technology was implemented in fabrication of tooth-retained restorations. This technology is now also used in the fabrication of implant abutments.24 The implant abutments which are designed and milled using this technology are known as CAD/CAM milled abutments.
In general, CAD/CAM milled abutments are made from a block of titanium or ceramic. An implant platform level impression may be required, depending on the manufacturers. Commonly, the implant platform impression is made and a working cast is fabricated. The cast is then scanned optically to generate exact 3-D images of the region. The information is sent to the milling machine to form the morphologically correct abutment from a block of titanium alloy.25 In another technique, a specially designed healing abutment, known as Encode Healing Abutment® (Biomet 3i), is used. These abutments have codes which are engraved onto their occlusal surfaces. The codes provide the computer with essential information, such as the hex position, implant platform and implant diameter, which is required for fabrication of the final abutment.12,25
The CAD/CAM technology allows elimination of certain factors, such as inferior accuracy of casting procedures that negatively affect the long-term success of the restorations. So the CAD/CAM milled abutments are more precise than those created using the traditional casting technique. They also have no porosity.12 Procera Abutment® (Nobel Biocare) is an example of CAD/CAM milled abutments.
The precision at the implant interface of gold-machined UCLA abutments and CAD/CAM milled titanium abutments were studied by Vigolo et al.24 No significant differences relative to rotational freedom were found among abutments obtained by the two techniques.24
The CAD/CAM technique seems promising and may replace the conventional techniques for implants in the near future.24 However, the use of the CAD/CAM milled abutments is expensive, which may preclude their wide use at present.17
Different abutment types are displayed in Figure 5. Table 3 summarizes the different abutment types, their trade names and manufacturers.
| Implant Type | Trade Name | Manufacturers |
|---|---|---|
| 1. Ready-made (Non-modifiable) | CeraOne/NobelActive/Snappy Abutment |
Nobel Biocare |
| 2. Ready-made (Modifiable) | CeraAdapt |
Nobel Biocare |
| 3. Custom-made (Metal) | UCLA (plastic pattern only)* |
Straumann |
| 4. All-ceramic | Procera alumina/Procera zirconia |
Nobel Biocare |
| 5. CAD/CAM | Procera |
Nobel Biocare |
It is not possible to identify one of the mentioned abutment systems as the ideal system for every case, as each of the mentioned systems has some advantages and disadvantages in different conditions. In other words, a particular abutment system may be the system of choice for a particular case, but not necessarily for all other cases. At this time the use of different systems hugely depends on the clinical case and the operator/laboratory technician's preference.
It may be concluded that the cement-retained method is a flexible technique suitable for most clinical situations. Furthermore, it is a technique that, to some extent, resembles the conventional crown and bridge procedure with which the dentist and the dental technician are familiar. However, the cement-retained restoration is difficult to retrieve as the restoration has to be cut and a new restoration made.
Among the five abutment types, the custom-made one seems to suit different clinical challenges, as it is easy to use, cheaper and can be adjusted and modified. Also, the laboratory procedure is similar to the conventional crown and bridge procedure. However, it is made of metal and, in many clinical situations, such as when a high aesthetic demand is required, an optimal result may be difficult to achieve.
The use of ready-made, non-modifiable metal abutments could be used for a posterior tooth in a non-aesthetic area, while their use is not ideal when restoring an anterior tooth in the aesthetic zone, as it causes tissue greying. When aesthetics is a major requirement, all-ceramic abutments may be used with a very good outcome.
The use of CAD/CAM abutments may shorten the laboratory procedure, save time and may eliminate some human errors. However, the CAD/CAM abutments are more expensive and have a shorter clinical history than the other abutment types. Nevertheless, this technique seems promising and may be used more widely in the future.
It is the authors' opinion that further long-term studies on different systems are still needed to aid the dentist when deciding on the use of a particular system