References
Multiple myeloma as a mandibular radiolucency – a difficult diagnostic challenge
From Volume 45, Issue 4, April 2018 | Pages 347-348
Article

Case report
A male patient with a non-vital lower left first molar was referred to an oral and maxillofacial department with a large radiolucency associated with the distal root. The tooth was non-vital but had no associated symptoms.
A biopsy of the lesion was undertaken. It was found to extend into soft tissue and was a friable mass of connective tissue, which histologically was confirmed to be a plasma cell tumour.
A 57-year-old male attended his general dental practitioner (GDP) for a routine examination with no presenting complaint. Multiple carious teeth were noted, including a lower left first molar (LL6) which had a full gold crown with deep distal secondary caries present. A periapical radiograph of the tooth revealed a radiolucency associated with the distal root, the extent of which went beyond the borders of the small film. The tooth itself was non-vital but there was no clear history of toothache nor any other painful symptoms. The lower left second molar had been extracted a number of years earlier. A provisional diagnosis of a cyst was made and the GDP referred the patient to the local Oral and Maxillofacial Surgery (OMFS) department for management.
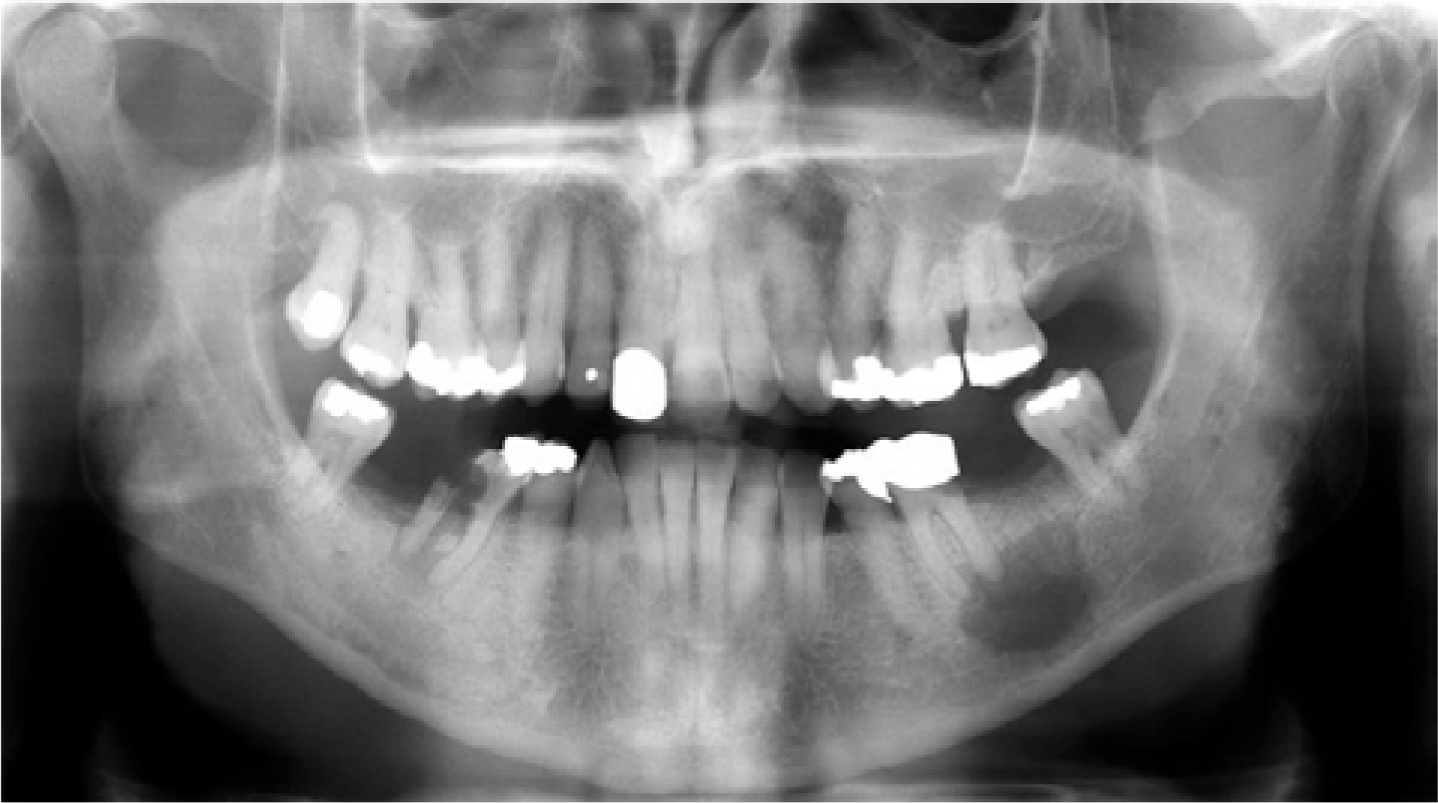
At the OMFS consultation a carious, non-vital LL6 was confirmed with ethyl chloride, however, no expansion of the mandible or swelling within the soft tissues was noted. The patient complained of no toothache, bone pain or neurological symptoms. An OPG radiograph (Figure 1) was taken which showed that the lesion was a unilocular radiolucency extending from the roots of the lower left first molar, distally to the healed site of the second molar, and inferiorly to the inferior alveolar canal.
The patient was noted to have significant medical problems. He had been diagnosed with multiple myeloma in 2009 which was managed with chemotherapy followed by an autologous bone marrow transplant, and was clinically in remission. His multiple myeloma had resulted in renal failure which left him requiring dialysis three times a week. He also received intravenous bisphosphonates. The patient was listed for general anaesthetic extraction of LL6 and enucleation/biopsy of the cyst.
No pre-operative CBCT was taken as, although the OPG suggested a close proximity to the inferior alveolar nerve, a buccal approach was planned for the biopsy which meant direct vision was possible to identify and avoid any vital structures. The patient was admitted on the day of surgery some 6 weeks later. His condition was unchanged except for a broken right radius following a fall 3 weeks previously.
Clinically, by this stage he had developed a non-tender fluctuant swelling which filled the buccal sulcus adjacent to the LL6. Observations were all within normal limits. The differential diagnosis for the swelling was an abscess cavity or tumour, including a brown tumour or multiple myeloma. As either condition would require a surgical approach in order to obtain tissue samples, the operation proceeded as planned and was covered with antibiotics.
A 2-sided muco-periosteal flap was raised under general anaesthesia. The mucosa was dissected free of the mass, which was followed onto the bone. There was a very large bony defect buccally from the LL4 region to the LL7 region. The lower extent of the lesion was difficult to access and was in extremely close proximity to the inferior alveolar nerve, so it was decided at this stage simply to de-bulk and send the tissue for histology. Once opened, the lesion was found to be brown, friable and highly suggestive of malignancy.
The lingual cortex had also been perforated by it. The LL6 was removed uneventfully and wound closure was completed. The patient was advised to remain on a very soft diet for 6 weeks and was discharged the same day.
The histopathology results showed the lesion to consist of fibrous stroma incorporating a small amount of bone which was extensively infiltrated by neoplastic cells which were barely recognizable as plasma cells. Immunohistochemistry was positive for VS38c, CD138, EMA, CD56 and AE1/3. Despite positivity for AE1/3 being unusual, the appearances suggested a plasma cell neoplasm, which fitted with a history of multiple myeloma.
Two weeks after the operation the patient was well in himself. He was informed of the diagnosis and the fact that it was almost certainly a recurrence of his multiple myeloma. He was referred on to the haematology-oncology service for bone marrow aspirate and further management. At that time orthopaedics also raised concerns that his wrist fracture may be pathological too. This has subsequently been confirmed. No further surgery on the mandibular lesion was deemed necessary given as the patient began another course of chemotherapy with the haematologists.
Discussion
Multiple myeloma is a cancer of the plasma cells. Plasma cells are a form of white blood cell, and produce antibodies. They are derived from B lymphocytes, and are their most mature form. Initially, patients with multiple myeloma are often asymptomatic, but can go on to develop bone pain, anaemia, renal impairment, bleeding problems and frequent infections. The plasma cells can form masses either in bone or in soft tissue. When only one site is involved, this is termed a plasmacytoma. Cases with multiple sites are designated multiple myeloma.
Diagnosis is based on blood and urine findings and bone marrow aspirate will also demonstrate the cancerous cells. Patients may have ‘CRAB’ features:
It is a treatable condition, using combinations of steroids, chemotherapy and bone marrow transplantation. Bisphosphonates are used for bone pain and control of serum calcium levels. Radiotherapy can also be used for bone pain. Whilst it is treatable and controllable for a time, it is generally incurable.
It is extremely rare for patients to present with isolated deposits of multiple myeloma in the mandible. A review of the literature in 2015 showed only 14 cases had been described. Goetze et al presented an osseous plasma cell neoplasm in the mandible and found 13 other cases in the literature over the last 30 years.1 Interestingly, they found that most cases presented with swelling, but pain was an inconsistent feature, making its use as a differentiating feature questionable. They presented with unilocular or multilocular lesions, again not helping diagnostically, unless a multilocular lesion was present, when you would naturally be more suspicious of a sinister cause.
We report this case as an example of a rare presentation of a relatively common disease, which presented diagnostic difficulties. This mandibular radiolucency could easily have been mistaken for a radicular cyst or spreading dental abscess. Without surgical investigation and histopathology, it was impossible to diagnose as the patient lacked the key features of both diagnoses; he had no bone pain or sensory changes, but equally he had no dental symptoms or signs of significant abscess formation (pain, pyrexia, trismus). A careful approach allowed preservation of the inferior alveolar nerve whilst debulking the lesion and obtaining sufficient material for a diagnosis to be made.
Conclusion
General dentists should be aware of myeloma, that it can cause bleeding problems in the patient, increased susceptibility to infection, that the patient may be on bisphosphonates, and that it is a rare but known cause of mandibular radiolucencies.
