References
To retrieve or not to retrieve the coronectomy root – the clinical dilemma
From Volume 40, Issue 5, June 2013 | Pages 370-376
Article
Coronectomy is now being proposed as a treatment option for mandibular third molars deemed on radiographic assessment to be at risk of inferior dental nerve injury. However, there is understandable concern amongst clinicians, who are sceptical of the value of the technique, as a root is retained in the socket and with it lies the prospect of late complications, such as infection. Furthermore, the fact that a retained root remains in the socket may cause a diagnostic issue if the surgical site remains symptomatic and may lead to other causes being overlooked. In the presence of rather non-specific symptoms, the dilemma is whether they arise from the retained root or were just a consequence of the surgical procedure. In the former instance, the root should be retrieved but may still carry the risk of injury to the IDN. Post coronectomy patients are likely to be encountered more frequently by GDPs as the technique becomes more popular. It is therefore prudent that GDPs have some knowledge of the common causes of symptoms post-coronectomy and their optimum management. In this paper, the authors share their expertise based on experience gained from coronectomy procedures undertaken at Guy's Oral Surgery Department.
Common sequelae of coronectomy
Patient group
The surgical unit at Guy's Dental Hospital has adopted coronectomy as an effective method of protecting the IDN from injury. In the period of 2005–2012 over 2500 teeth have been treated by this technique. The experience gained informs the current discussion.
Coronectomy was carried out under all modalities of anaesthesia (LA, IV and GA) and by three grades of clinicians (Consultants, Specialist Registrars and Specialty Dentist). Patients were originally assessed clinically and with a dental panoramic radiograph. Based on radiological findings (mandibular third molar root crosses the IDN canal), a subgroup of patients considered at increased risk of IDN injury was selected for coronectomy. The coronectomy technique used in the study was that described by Gleeson et al.1 Those patients who were not reviewed routinely were given clear instructions to return if they had persistent problems following treatment. In the past 18 months, the department has retrieved 10 coronectomy roots for a number of different reasons that are discussed below.
The technique of coronectomy has the specific advantage in that it almost eliminates inferior dental nerve injury. However, the retained mandibular third molar roots can introduce new clinical and diagnostic problems. They arise when the patient either experiences a standard complication of surgery or remains symptomatic post-surgery. The question is whether the retained root is a causative factor. Persistent signs and symptoms of an infected root should be treated appropriately by extraction, however, in our experience, this is an uncommon finding in coronectomy patients if the original procedure was carried out on a pathology-free mandibular third molar as per the guidelines on this technique. A management dilemma arose in a number of discrete clinical scenarios presented below.
Alveolar osteitis
Alveolar osteitis (AO) is a well-known sequelae of both forceps and surgical extraction of molar teeth. The frequency of AO for mandibular third molars ranges from 0.3–26%2-11 and also occurs after coronectomy,11-15 with a reported incidence of 2%14–12%.13
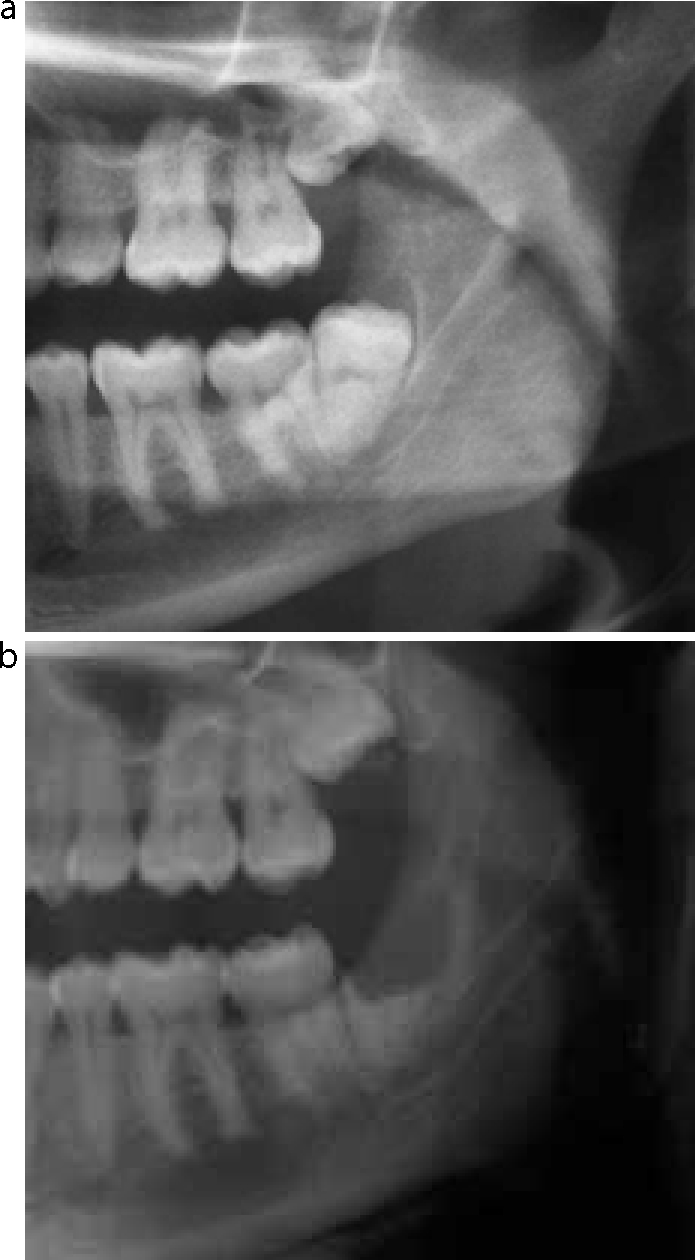
Current experience suggests that post-coronectomy AO does not jeopardize the outcome of the coronectomy procedure. Despite the fact that the socket is bare and usually filled with food debris, the retained root is unaffected. This is surprising but evidence suggests that the root retains its vitality. If primary closure had been achieved and appears to be maintained with symptoms of AO, then the distal aspect of the second molar should be checked with a periodontal probe. Usually a dehiscence is found behind the crown, confirming the diagnosis of an AO socket. Unless there is evidence of gross infection, then the site can be managed in the normal way by thorough irrigation with saline or chlorhexidine and the socket dressed with Alvogyl (butyl aminobenzoate, eugenol and iodoform). The patient is instructed to irrigate the socket by way of a Monojet SyringeTM and the Alvogyl dressing may have to be repeated. Most cases of post-coronectomy AO settle (Figure 1) with repeat dressing. Root retrieval is not normally required.
Draining sinus tract
A minority of patients may complain of ongoing discomfort when the socket has healed. On occasions this is due to a small sinus tract running from the root to the oral cavity. It can be revealed by a buccal infiltration of local anaesthesia which flushes debris or non-clear fluid from the sinus (see ‘Infection’). The condition usually occurs more than six months after coronectomy. If a sinus tract is present with clinical symptoms, this is an indication for root retrieval. From the ten roots retrieved, seven were due to clinical signs and symptoms of a low-grade chronic infection. From these seven, five were seen to have partially erupted through the mucosa, which explained the symptoms. Radiographically, there was no suggestion of apical pathology related to any of the roots. Four of the seven roots retrieved were sent for histological examination which demonstrated normal, non-inflamed healthy pulp. The draining sinus is therefore likely to be a low grade chronic soft tissue or periodontal infection and not related to a non-vital coronectomy root.
Root migration
Migration of the retained roots has been reported in most coronectomy studies.12,13,16-19 All patients should be warned of this phenomenon. The root may eventually erupt harmlessly to the mucosal surface.
Current experience indicates that most roots migrate away from the IDN along the long axis of the root, but it is not inevitable (Figure 2). Initially (first 3 months), migration may be rapid and then cease or continue gradually over time. Neither migration nor eruption are indications for surgical intervention unless the roots reach the mucosal surface and become symptomatic.
Apical radiolucency
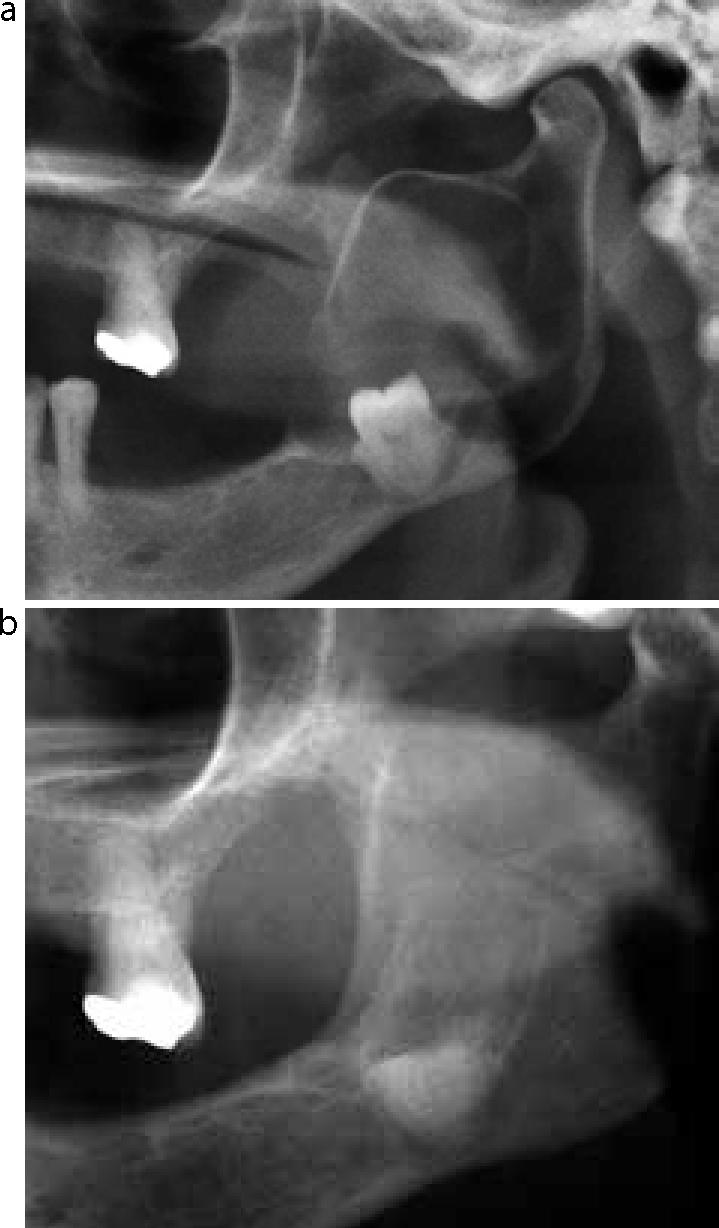
‘Apical radiolucency’ is a phenomenon restricted to coronectomy. It is seen in the majority of patients, especially in the first three months post-surgery. As the root migrates away from the IDN canal a darkened area remains below the root and may erroneously be interpreted as apical pathology. If the pre- and post-surgery radiographs are examined closely then the radiolucent area matches the outline of the root prior to migration. The radiolucent area or migration-lucency zone represents delayed regeneration of bone behind the moving root and is not infection (Figure 3). The migration-lucency zone is not an indication for root retrieval.
Enamel lipping
Despite the fact that sectioning of a tooth seems a straightforward procedure, the technique of coronectomy is not always easy to perform. The intention is to retain as much buccal bone as possible and at times this may limit access to the root. This arises particularly with the disto-angular third molar where the mid third to apical portion of the root is in contact with the adjacent second molar. Traditional extraction can leave an exposed root surface or potential deep periodontal pocket, which can lead to a guarded long-term prognosis for the second molar. Coronectomy can eliminate this risk by maintaining the bone (Figure 4) but restricted access can result in enamel lipping. The latter occurs when the fracture line (fissure bur cut followed by couplands elevator) leaves a shard of enamel attached to the periphery of the root. This occurs particularly with disto-angular impactions, when the fissure bur is kept away from the distal aspect of the adjacent lower second molar for fear of inadvertently damaging the tooth.20 Another risk is the mesio-lingual corner of a mandibular third molar following decoronation. The cause is an inadequate fissure cut into the crown of the tooth that results in a retained shard of enamel. This should be burred down together with the root surface to a position 3 or 4 mm below the surface of the bony crest, but is not always easy to accomplish owing to the limitations in access. Enamel has no blood supply and is treated as a foreign body by the local tissues. It acts as an irritant to the soft tissue and the socket will not heal adequately. The enamel lip is usually visible on radiographic examination (Figures 5 and 6). The clinical picture is similar to a dry socket but does not resolve with adequate treatment. Enamel lipping leading to a non-healing socket should be considered for root retrieval.

Acute infection
Infection of the retained root is uncommon. Pus extruding from the socket rather than pain is an indication for root retrieval. A Cone Beam CT (CBCT) may be required for surgical planning. Over the last 18 months, no root has been removed for reasons of acute infection.
Associated pathology
Some impacted mandibular third molars are associated with odontogenic cysts and coronectomy is not necessarily excluded in this situation. Dentigerous cysts originate at the amelo-dentinal junction and so decoronation will eliminate the source of the pathology and allow the root to remain safely in situ (Figure 7). The situation where this form of management is optimum is in the presence of a large dentigerous cyst where the integrity of the mandible is at risk if the tooth is removed and/or there is a significant risk of inferior dental nerve injury. Leaving the root in situ maintains the strength and integrity of the mandible.20 Care must be taken to select cases carefully and to avoid keratocysts or cystic ameloblastoma, where this approach is incorrect. Routine follow up at six-monthly intervals will show bone healing and, unless symptoms specific to the root arise (as discussed above), root retrieval is not required.
Pain
Post-coronectomy, symptoms of pain can be difficult to interpret. Experience shows that, since the patient knows a tooth fragment is still present in the socket, he/she is alert to potential complications and has a low threshold for complaints. Post-operative pain lasting up to 10 days is unremarkable following routine removal of a mandibular third molar. The same applies for coronectomy. Sustained symptoms (1–3 months) should be investigated through history, full clinical and radiographic assessment. Most patients will fall into one of the aforementioned diagnostic categories.
Persistent complaints pressurize the clinician to remove the root and the decision is simple if the root has safely migrated away from the inferior dental nerve canal. If not, management has to be guided by clinical judgment. In those patients who have continual complaints post-surgery, the original diagnosis should be revisited. The incidence of symptoms post coronectomy are generally low.
Conclusion
Coronectomy is slowly emerging as a realistic alternative to mandibular third molar extraction in those patients judged at risk of IDN injury. The elective retention of the root remains a source of contention regarding its long-term outcome, prognosis and safety. Our experience is that root retrieval post coronectomy is a rare occurrence, as generally the roots remain asymptomatic. Consequently, if non-specific symptoms persist, a full assessment is advised before further surgery is contemplated.
