References
The impact of medication on the periodontium: a review of the literature
From Volume 45, Issue 3, March 2018 | Pages 256-265
Article

Periodontal disease is a complex inflammatory disease that affects the soft and hard periodontal structures; including the gingivae, cementum, periodontal ligament and alveolar bone.1 Periodontal disease is plaque-related2 and initiated by bacteria, with the clinical determinants of host response and genetic environmental risk factors influencing the severity and extent of disease.3,4,5,6
Although the main aetiology of periodontal disease is poor oral hygiene and the presence of dental plaque, certain medications can exacerbate existing periodontal disease. Phenytoin, cyclosporine and calcium-channel blocking antihypertensive drugs are the most commonly quoted drugs related to gingival disease; however, other medications can have an adverse effect on the periodontium, especially in the presence of suboptimal oral hygiene (Table 1).7,8,9,10
| Drug-influenced gingival diseases |
Medications
Medications affecting the periodontium, summarized in Table 2, can be classified into four categories and are:
| Effect on Periodontium | Medications |
|---|---|
| Xerostomia | Antihypertensives |
| Predisposition to gingival bleeding | Anti-coagulants (Warfarin) |
| Possible reduction of bleeding on probing | Corticosteroids |
| Drug-induced gingival overgrowth | Anti-convulsants |
| Increased expression of periodontal disease | Oral contraceptives |
| Discoloration of gingival tissues | Tetracyclines |
| Reduced alveolar bone density | Corticosteroids |
| Medication Related OsteoNecrosis of the Jaw (MRONJ) | Bisphosphonates |
Medications affecting oral health
Xerostomia is a common side-effect of certain medications and is related to increased plaque accumulation, which in turn increases the risk of periodontal disease and caries.12 The most common medications causing xerostomia are antihypertensives (including diuretics, angiotensin converting enzyme inhibitors and calcium channel blockers), antidepressants, sedatives, centrally acting analgesics, anti-parkinson medication and anti-allergy medication.13
Medications affecting periodontal disease diagnosis
Bleeding on probing is a sign of active periodontal disease. Anti-thrombotic agents, including anti-coagulants (eg Warfarin), anti-platelet agents (eg clopidogrel), and non-steroidal anti-inflammatory drugs (NSAIDs) (eg Aspirin) can predispose patients to gingival bleeding.11 Additionally, herbal remedies with ginger or garlic may be associated with false positive bleeding on probing.11 On the other hand, corticosteroids and antibiotics have the potential to reduce bleeding on probing and underestimate existing periodontal disease.14
Medications affecting gingival and oral mucosal tissues
Phenytoin, Cyclosporine and certain calcium channel blockers (eg Nifedipine, Amlodipine, Verapamil, Diltiazem, Isradipine) are related to gingival enlargement,7,8,9 with prevalence of 50%, 30% and 10%, respectively.9,15,16 In addition to these, oral contraceptives and hormone replacement therapies have been associated with increased expression of periodontal disease.17,18 Prednisolone and Azathioprine may possibly offer protection against gingival enlargement in organ transplant patients, but good oral hygiene is still a prerequisite.19 A strict oral hygiene regimen will aid prevention of gingival enlargement and is the most important element of gingival health.20,21
Medications affecting alveolar bone
Minocycline, a semi-synthetic type of tetracycline used to treat acne, rosacea and rheumatoid arthritis, can cause black pigmentation of the gingival tissues, teeth and the underlying alveolar bone.22 The mechanism of bone pigmentation is not entirely clear, however, owing to its lipophilic nature, minocycline has extensive tissue penetration and ability to bind to collagen. Subsequent degradation/oxidation results in the grey/blue deposit which discolours the bone.23 Pigmentation is more likely to occur with doses exceeding 100 mg and when used for over a year.
Systemic corticosteroid use is associated with reduced alveolar bone density24 and increased susceptibility to bone loss in pre-existing periodontal disease. Antibiotics and NSAIDs prevent bone loss but the evidence for their use in treatment is inconclusive.25
Anti-resorptive medications including bisphosphonates (Alendronate, Zoledronate) and RANK ligand inhibitors, such as the mono-clonal antibody Denosumab (Xgeva®, Prolia®) are used in management of patients with osteoporosis, Paget's disease of bone and bone metastases.26 The mode of action is mainly through direct inhibition of osteoclastic function, thus preventing bone resorption and remodelling. The systemic effect of generalized increased skeletal bone density of such medications also benefits the alveolar bone but increases the risk of Medication Related OsteoNecrosis of the Jaw (MRONJ),27,28 with increased risk through intravenous administration.26 MRONJ is characterized by exposed alveolar bone, tooth mobility, non-healing ulcers and idiopathic soft tissue infections. Animal and human studies undertaken to establish the effect of anti-resorptive medications on the periodontal tissues have shown varied outcomes. Prevention or reduction in bone resorption in plaque-induced periodontitis has been observed, however, other studies show an increase in periodontal tissue destruction. Therefore, due to the low level of evidence, the use of such medications in the foreseeable future as an adjunct to non-surgical periodontal therapy is unlikely and a more robust evidence base is needed.29
Prescribers of bone anti-resorptive medication need to ensure that the patient undergoes a thorough dental examination to identify and treat any pre-existing oral disease prior to commencement of taking the medication. Teeth of poor prognosis should be removed and patients educated on the importance of good plaque control and regular dental examinations. Prevention of dental disease is important for these patients, as future extractions or surgery may carry a risk of MRONJ.
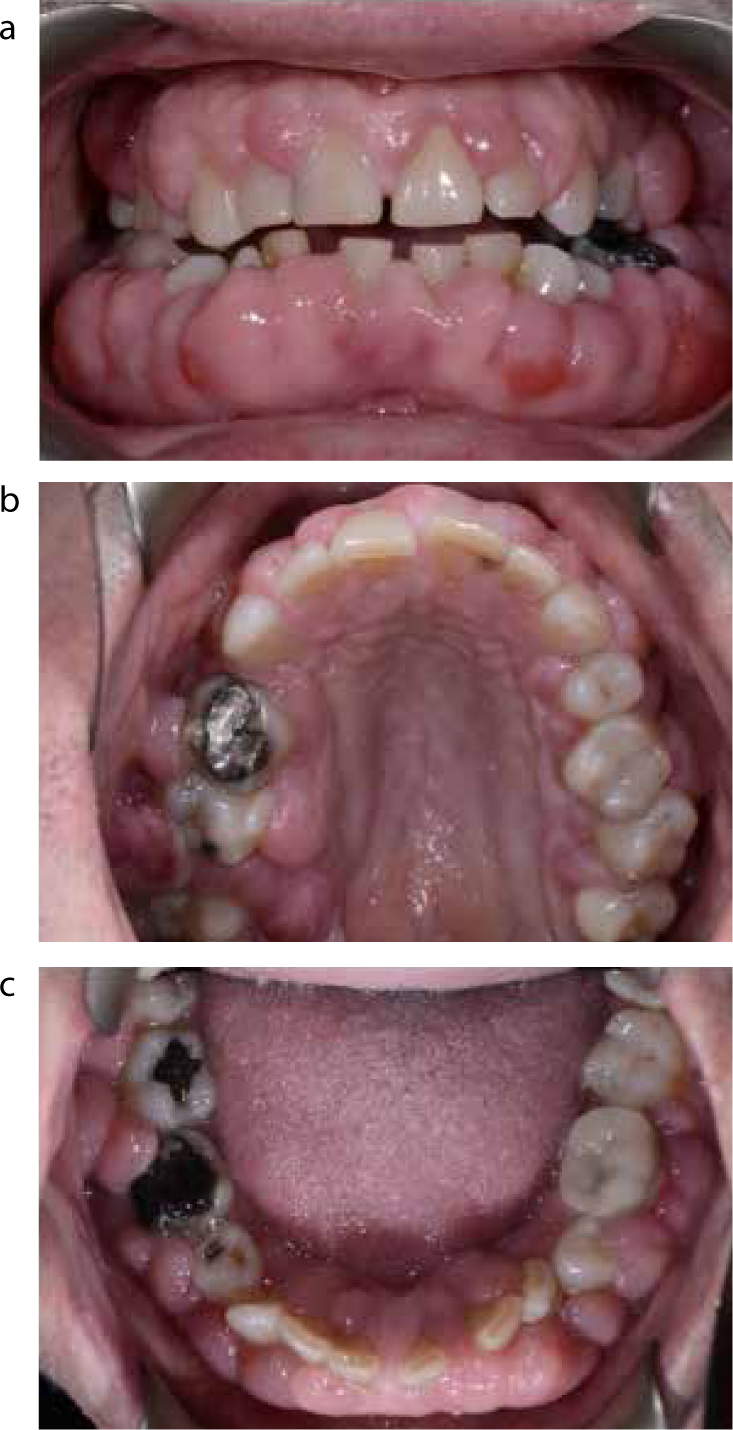
Drug-induced gingival overgrowth
Irrespective of the causative medication, the clinical appearance of drug-induced gingival overgrowth remains the same, with the onset usually occurring 1–3 months following commencement of the medication.30,31The dosage of medication, combined with the amount of dental plaque and periodontal inflammation, is linked to the prevalence and severity of the overgrowth seen.30
The anterior gingiva is one of the most commonly affected sites. The overgrowth begins normally in the interdental papilla region and spreads to cover the buccal and palatal surfaces of the teeth.31
Although largely a cosmetic concern, due to the overgrowth causing a reduction in clinical crown height and, in some cases, completely obscuring the teeth;30 the enlargement can also cause speech and masticatory difficulties,30,32 especially in young children.32 Fibrosis can occur in chronic overgrowth cases, leading to tooth migration and possible secondary malocclusions in the presence of altered masticatory habits.32 Enlargement of the interdental papillae can also lead to displacement of teeth and resulting diastemas.30
Although the gingival enlargement is not directly harmful, inflammatory changes become apparent due to the difficulties in plaque control; leading to oedema, erythema and bleeding. This appearance is commonly encountered in the presence of pre-existing periodontal disease.30
Patients with gingival overgrowth may be at an increased risk of periodontal disease, as well as tooth decay. Gingival overgrowth creates pseudo-pocketing coronal to the cement-enamel junction, which may hinder effective plaque control. In periodontally susceptible patients, this may progress to loss of periodontal attachment.32
Management
Non-surgical management
Due to the presence of false pocketing in cases of gingival overgrowth, it is important to ascertain if there has been any periodontal bone loss through appropriate radiographic examination, thus determining the presence of underlying chronic periodontal disease, which will require appropriate treatment.30
Preventive measures are by far the mainstay of treatment for gingival overgrowth and high standards of plaque control need to be achieved in order to control the level of any superimposed inflammation.30,32 Intensive tailored oral hygiene instruction33 should be demonstrated, with special attention to subgingival and interdental plaque removal. Adjunctive use of chemical plaque controlling agents, such as essential oil,32,34 cetylpyridinium chloride and chlorhexidine mouthwashes may be beneficial. There is evidence that chlorhexidine used at concentrations of 0.1% or 0.2% can reduce the severity of drug-induced gingival overgrowth when used adjunctively to mechanical oral hygiene measures.34
However, there should be caution in long-term use of chlorhexidine rinses as unwanted side-effects may occur, including brown discoloration of tooth surfaces and mucosa, taste disturbance and, more seriously, mucosal erosion, desquamative gingivitis and parotid swelling.35 Thorough deposit removal with scaling and root surface debridement should be undertaken alongside removal of plaque retentive factors, as necessary. Surgical intervention may need to be considered if primary local measures alone do not aid resolution.30,32
Substitution of the causative medication
Potential for overgrowth is something that the patient's medical practitioner should consider prior to prescribing; whilst effective management of established overgrowth lies mainly with the patient's dental professional.33
Gingival enlargement is a significant side-effect for some patients, using medication including phenytoin, vigabatrin and primidone for epileptic control.36 Valproic acid has a lower incidence of gingival enlargement and may be an alternative to phenytoin,37 although patients may be reluctant to consider changing medication where their condition has been under long-term control.
Immunosuppressant medication is used to protect against organ transplant rejection and is also used for management of conditions, including multiple sclerosis, rheumatoid arthritis, and dermatological disorders, including psoriasis and vesiculo-bullous disorders. Hypertension is a known side-effect of cyclosporin therapy38 and studies have confirmed increased risk and severity of gingival enlargement when immunosuppressant medication is taken alongside calcium channel blocker antihypertensive medication.37
Changing medications to those that do not cause gingival enlargement may be beneficial, with evidence of a 40% recurrence rate after surgery, if medication is not altered.39 Any suggested change should be communicated with the patient's medical practitioner, who will consider any adverse risks to the patient's general health;32 in which case the local risk of gingival overgrowth may not be as significant.30 In most cases, medication can be safely changed.
Tacrolimus is increasingly used as an alternative immunosuppressant to cyclosporine, which does not carry the same risk for gingival overgrowth,40,41 with additional advantages of improved cardiovascular risk profile, superior renal function and reduced hypertensive side-effects.42,43 Finally, Angiotensin Converting Enzyme (ACE) inhibitors have been suggested as an alternative to nifedipine, whilst maintaining a similar efficacy and less risk of gingival overgrowth.34
Pre-operative post-operative views of drug-induced gingival overgrowth cases are given in Figures 1 and 2.
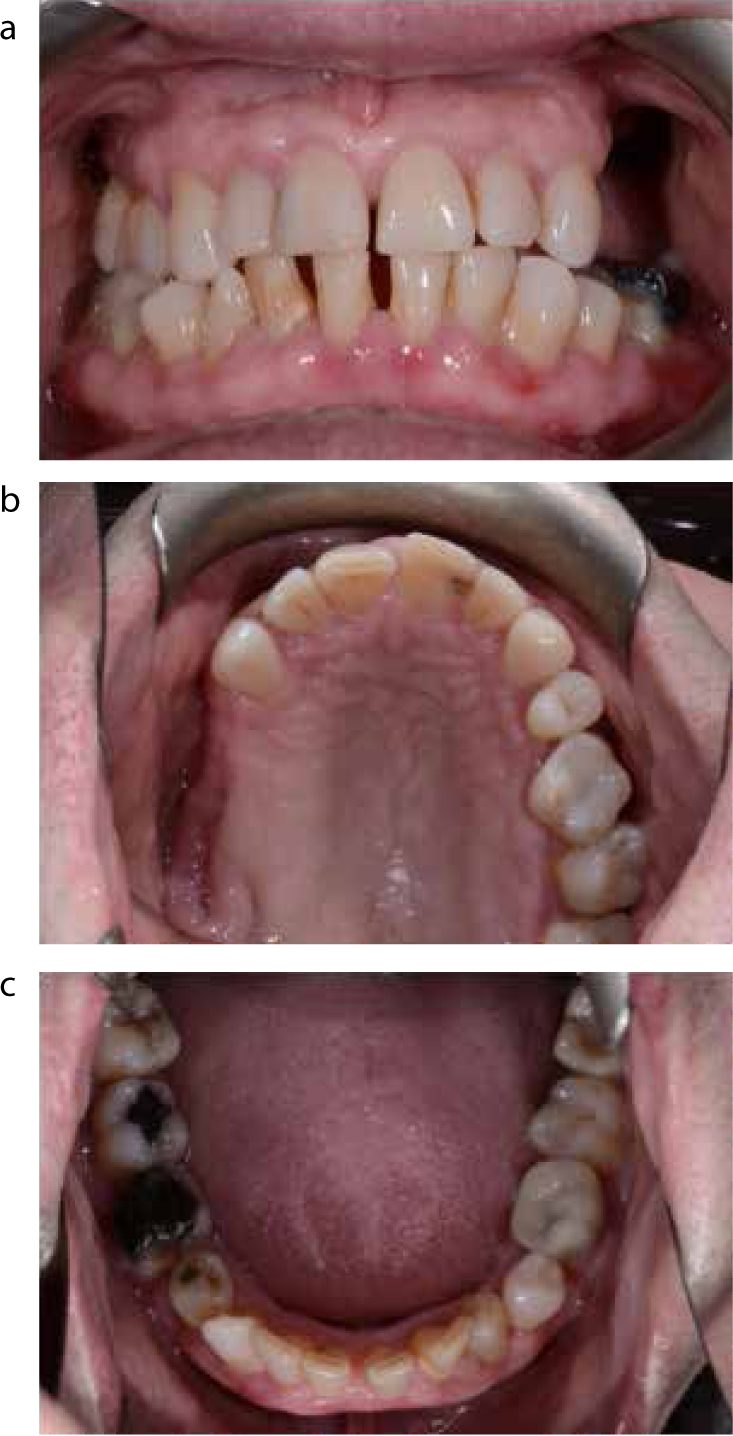
Surgical management
Where gingival overgrowth is significant, a surgical approach may be required to restore function and aesthetics, however, recurrence post-operatively is possible.39
Various surgical methods exist, including reduction and removal of the enlarged gingival tissues by gingivectomy, periodontal flap surgery, laser excision or electrosurgery.44 When histopathological examination of excised tissue is required, with confirmation of complete edge excision, this may best be achieved with conventional blade surgery. Conventional gingivectomy procedures may be carried out using an external bevel technique, however, total or partial internal bevel gingivectomies reduce post-operative complications but require greater technical skill.
The most widely recognized complications of gingivectomies are post-operative pain and bleeding, which may be reduced with laser or electrosurgery excision techniques. However, tissue necrosis can be a side-effect of electrosurgery, and may adversely affect the aesthetic outcome.45
Laser excision provides a superior incision margin and improved wound healing due to a coagulated layer along the incision, as well as a reduced incidence of scarring, and may be beneficial in less co-operative patients and for patients with medical contra-indications to conventional surgery, such as those with bleeding/coagulation disorders.45,46
The use of systemic medications to treat gingival enlargement
Systemic use of the macrolide antibiotic azithromycin has been reported to show improvement in gingival overgrowth,47 however, metronidazole31 and clarithromycin, from the same family of antibiotics, do not produce the same marked effect. A 3–5 day course of azithromycin has been shown to be efficacious in helping to manage cyclosporine-induced gingival overgrowth and does not affect the control level markers of serum ALT,48 creatinine or cyclosporine.40,41 The mode of action is unknown but is thought to reduce inflammation associated with the overgrowth,49 and through preventing collagen synthesis by blocking fibroblast cell proliferation.50,51 An alternative mode of action may be through an increase in gingival fibroblast phagocytic activity, which reverses the ability of cyclosporin-induced inhibition of collagen degradation, however, this phenomenon has not been reproduced in humans and is limited to animal studies.44 Evidence at present is weak and unproven,43 therefore further studies are required to determine the exact role of azithromycin in reducing gingival enlargement before it could be considered for mainstream use.47,48,49,50
The use of corticosteroid anti-inflammatory therapy in the treatment of gingivitis and other gingival conditions is equivocal and there appears to be no beneficial effect of systemic corticosteroid use on gingival inflammation, probing depths and recession.52
Conclusions
Patients are increasingly taking systemic medications that affect the health of periodontal tissues. Medical colleagues are becoming more aware of the importance of screening for, and treating dental disease, before prescribing medications or carrying out medical procedures, such as organ transplantation; requiring follow-up medication that may be long-term, or life-long, with a significant effect on the periodontal and other oral tissues. Dental professionals need an understanding of the effects of medication on the tissues and various modes of management of conditions that may develop as a result.
The foundations for good management are preventive advice with ongoing good oral hygiene and plaque control. This is essential for patients taking bone anti-resorptive medication where management of new dental disease may be problematical and carry the risk of MRONJ.
Gingival overgrowth can be managed with a non-surgical approach in the first instance, but may require surgery. However, in a large number of cases, liaising with the medical profession to substitute the causative medication, along with excellent plaque control, is key to preventing recurrence and repeated surgical procedures.
