References
Making sense of sensitivity
From Volume 40, Issue 5, June 2013 | Pages 403-411
Article

Every dentist will be aware of the recent increase in advertising for toothpastes to treat sensitive teeth. There are also a confusing number of products from which patients can choose (Figure 1). The wide range of treatment options available for dentine hypersensitivity indicates that there are many methods for managing this condition.

This paper reviews our current knowledge of dentine hypersensitivity (DHS) and describes the most commonly available products and treatment options.
A historical perspective of sensitive teeth
Dentine is a naturally sensitive tissue. When an otherwise harmless stimulus contacts freshly cut dentine, pain may be experienced. Historically, numerous attempts have been made either to reduce or eliminate this pain, by treating teeth with a wide variety of chemical remedies. These were generally unreliable, therefore operative dentistry continued to be very unpleasant. Fortunately, as local anaesthetic use became more common, the need for a desensitizing agent became less relevant. However, as dental health has improved and more people retain more teeth later in life, there has been an increasing need for a method to desensitize exposed dentine in otherwise healthy teeth.
Initially, the two most commonly used and now thoroughly researched ingredients were strontium and potassium. Sensodyne toothpaste was developed in the early 1960s, containing strontium chloride, but without fluoride, as these readily combine together as an insoluble compound with no clinical benefit. Macleans Sensitive was developed in the 1980s, with strontium acetate and fluoride, which were much less reactive.
In the 1970s, the desensitizing effect of potassium nitrate was discovered and, soon after, Sensodyne-F was developed as the first desensitizing fluoride toothpaste.
An excellent review of the development of strontium and potassium toothpastes was written by Markovitz.1
It is certainly challenging to consider any benefit that humans derive from having sensitive dentine, other than to provide evidence that there is something wrong with the tooth, such as a carious lesion. Yet, in evolutionary terms, the recognition that there was ‘something wrong’ occurred many thousand years before dentistry was performed that could manage these problems.
The concepts of dental pain and dentine sensitivity have also been a longstanding curiosity for dentists. In 1959, Robert Cutler wrote a letter, published in the British Medical Journal, entitled ‘Mysterious dentine’.2 This began:
‘To the practising dentist not wholly bogged down with the mechanical procedures in the mouth, the symptomatology of tooth pain presents a continued fascination.’
Forty years later, Martin Addy co-authored an excellent review article in the British Dental Journal, the title of which highlighted the curiosity that DHS continued to hold for dentists3 – Dentine hypersensitivity – an enigma?
What is dentine hypersensitivity?
Dentine hypersensitivity is characterized by a short sharp pain arising from exposed dentine in response to stimuli, typically thermal, evaporative, tactile, osmotic or chemical and which cannot be ascribed to any other form of dental defect or disease.4
Data regarding the prevalence of DHS are inconsistent but tend to range from 3.8%5 to 35%6 in the general population and self-reported sensitivity ranges from 37% to 52%.7
There is a higher reported prevalence in females, in patients between 20–40 years, patients with recession or undergoing therapy for periodontal disease (up to 98%),8 bulimics, xerostomics and tobacco chewers.9
There are conflicting reports on which teeth are most commonly affected by DHS. It is, however, clear that the buccal-cervical margins of all teeth, as the most prominent surfaces, are most likely to be involved.
How does dentine hypersensitivity occur?
Dentine is normally insulated by enamel, cementum and the periodontium. Enamel can be lost by caries, toothwear, trauma and dental treatment. Dentine becomes exposed either by loss of enamel or gingival recession (Figure 2).
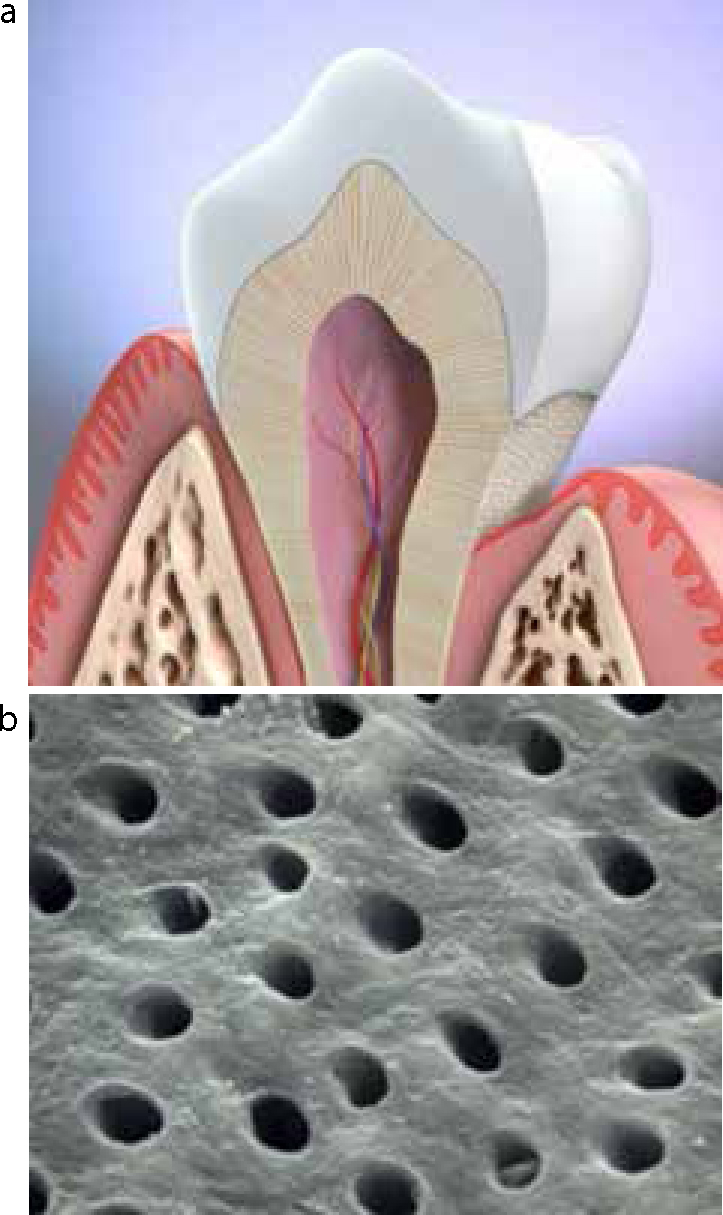
If the surface openings of the dentine tubules are patent, the unpleasant sensation of DHS can occur when external stimuli are applied to those areas of the tooth. It is recognized that teeth with more patent tubules per unit area are more likely to be sensitive.10
Exposed dentine is usually covered with a smear layer and this natural insulator prevents DHS. The smear layer is a tenacious layer of organic and inorganic material, up to 50 µm thick, that adheres to the tooth surface and penetrates into the dentine tubules. In the absence of a smear layer, the dentine tubules may be blocked by calcium phosphate, formed from saliva. Therefore, for DHS to occur, the smear layer and the deposits of calcium phosphate will have been removed, by either mechanical or chemical means.
Several mechanisms have been proposed to explain how stimulus at the dentine surface leads to the sensation of DHS. However, the most widely accepted is the Hydrodynamic Theory. This was initially proposed by Alfred Gysi in 190011 and was then investigated and reported by Brännström, whose name is most often associated with this mechanism, in 1963.12–14 This postulates that external stimuli, such as temperature, can alter the flow of fluid within the exposed dentine tubules. This flow leads to a pressure change within the tubule which is detected by sensory A-delta fibres within the pulp, resulting in a short, sharp pain.
Management of dentine hypersensitivity
Prevention
Patients will have developed DHS by either physically or chemically exposing the patent dentine tubules. Therefore, any management strategy should have a clear preventive message alongside the treatment provided.
Gingival recession
As DHS is frequently associated with recession on the prominent buccal and labial tooth surfaces, it is clear that the common ‘scrubbing’ action of toothbrushing is harmful (Figure 3). Patients should be instructed to use a toothbrush with medium bristles, to hold it between the fingers and thumb in a ‘pen-holder grip’, rather than in the usual ‘screwdriver’ grip and to employ a circular action when brushing.

Chemical erosion
The role of acidic foods and drinks in tooth erosion is now well understood and dental clinicians will frequently recognize these effects on their patients' dentitions (Figure 4). As these products soften enamel and enable its removal by attrition and abrasion, along with loss of the dentine smear layer and any calcium phosphate deposits that are occluding the tubules, it is essential that appropriate dietary advice is given.

In particular, the frequency of acidic food and drinks and the importance of a delay before toothbrushing should be explained. It is appropriate to encourage the patient to record a diet history that will identify the erosive components in the diet.
Tooth whitening
Of patients having bleaching procedures, 70% experience short-term temperature sensitivity, regardless of the method used. It is known that hydrogen peroxide may penetrate through the tooth to the pulp, resulting in an inflammatory reaction. Whitening also removes staining, which can increase the patency of the dentine tubules.
Patients commencing tooth-whitening procedures should be warned of the likelihood of DHS. If it occurs during home whitening, they should wear their trays less frequently, for example either on alternate nights or for shorter time periods. It can be helpful for patients to use desensitizing toothpaste in the trays, when not using the bleaching agent.
Treatment
Most treatments for DHS take one of two forms:
Reducing the pulpal nerve response
A nerve cell has more potassium ions inside and more sodium ions outside the cell membrane. If additional potassium ions are flooded around the cell, they are pumped through the cell membrane and the cell is less able to activate in response to stimulus. Therefore, treatments that increase the potassium ion concentration within the tubules and pulp tissues and then maintain the higher concentration can reduce the pulpal nerve response and lessen the problem of DHS. On the basis of this effect, numerous toothpaste products have been developed, containing one of a variety of potassium compounds (Table 1).
| Pottasium Ingredient | Tooth Product | Fluoride |
|---|---|---|
| 5% potassium nitrate | Sensodyne Total Care Gel | 1450 ppm |
| Sensodyne Total Care F | 1400 ppm | |
| Sensodyne Total Care Gentle Whitening | 1400 ppm | |
| Sensodyne Total Care Extra Fresh | 1400 ppm | |
| Sensodyne ProNamel | 1450 ppm | |
| Sensodyne ProNamel Gentle Whitening | 1450 ppm | |
| Sensodyne Multi Action Iso Active | 1450 ppm | |
| Sensodyne Whitening Iso Active | 1450 ppm | |
| Colgate Sensitive Enamel Protect | 1100 ppm | |
| Colgate Sensitive Multiprotection | 1500 ppm | |
| 3.75% potassium chloride | Sensodyne Gum Protection | 1400 ppm |
| 5.5% potassium citrate | Colgate Sensitive Fresh Stripe | 1500 ppm |
However, it is recognized that this method of treatment is not as effective as hoped. Potassium-containing toothpastes can lead to decreases in dentinal hypersensitivity in response to various stimuli but take at least two weeks, of twice daily use, to become effective and the greatest reductions may not be achieved for eight weeks. However, a review of randomized controlled trials in this area, carried out by the Cochrane Collaboration, concluded: ‘….no clear evidence is available for the support of potassium containing toothpastes for dentine hypersensitivity.’15
Yet such toothpastes remain popular with consumers and manufacturers alike, probably as consumers recognize and trust well-known brand names, almost regardless of the active ingredients. Manufacturers continue to produce these toothpastes, despite significant marketing efforts with their other products, which are clinically proven to be more effective. The toothpastes also have additional patient benefits, as a result of other active ingredients.
In the UK, the two main desensitizing toothpaste ranges are made by GlaxoSmithKline GSK (Sensodyne) and Colgate Palmolive. There are currently nine forms of potassium-based Sensodyne toothpastes, including two forms of Sensodyne ProNamel. Colgate Palmolive has three potassium-based toothpastes available. Other well-known brands such as Crest, Macleans, Beverley Hills, Oral-B, Aquafresh and Arm and Hammer also produce potassium-based toothpastes.
Occluding the dentine tubules
As a natural dentine smear layer is effective at preventing DHS for most patients, it is appropriate that treatments exist to create an artificial smear layer. These can either be used by the patients themselves, again in the form of a toothpaste, or alternatively as a professionally applied product in the dental clinic.
Toothpastes for use at home
In recent years, GSK and Colgate Palmolive have separately developed and thoroughly researched new toothpastes that are able to occlude the tubules reliably and create a smear layer.
Colgate Palmolive has widely publicized the immediate and lasting benefits of Pro-Relief toothpaste, which uses ‘Pro-Argin technology’. This contains calcium carbonate and the amino acid arginine, which combine together to seal and plug the open dentine tubules.
GSK has made similar statements for Sensodyne Rapid Relief, which contains strontium acetate. GSK has also developed Repair and Protect, which uses ‘Novamin technology’. Novamin is a calcium sodium phosphosilicate compound which releases calcium and phosphate ions when it comes into contact with water or saliva. These ions bind to the exposed dentine surface, forming a strong, protective and acid-resistant layer.
A series of papers has been published in special editions of the Journal of Clinical Dentistry to explain the development and support the effectiveness of these new products.16–22
As with potassium-based toothpastes, other well-known brands such as Macleans, Crest, Oral-B and Arm and Hammer also produce toothpastes that occlude tubules and create a smear layer (Table 2).
| Occluding Ingredient | Toothpaste Product | Fluoride |
|---|---|---|
| Strontium chloride | Sensodyne Original | 0 |
| Strontium acetate | Sensodyne Rapid Relief | 1040 ppm |
| Calcium sodium phosphosilicate (‘Novamin’) | Sensodyne Repair and Protect | 1450 ppm |
| Pro-Argin technology' |
Colgate Sensitive Pro-Relief | 1450 ppm |
| ‘Pro-Argin technology’ |
Colgate Sensitive Pro-Relief + Whitening | 1450 ppm |
| ‘Pro-Argin technology’ |
Colgate Sensitive Pro-Relief Multi-Protection | 1450 ppm |
| Strontium acetate | Macleans Sensitive | 1040 ppm |
| Stannous fluoride | Crest® PRO-HEALTH® Sensitive + Enamel Shield | 1040 ppm |
| Stannous chloride | Oral-B Pro Expert Sensitive + Gentle Whitening | 1450 ppm |
| Soluble Calcium citrate (‘Liquid Calcium’) | Arm and Hammer Enamel Care | 1100 ppm |
Patients with DHS will want a toothpaste product with the following properties:
They will understandably be confused by the numerous products available and it is likely that most dental professionals would struggle to make an informed choice of product, based on the available evidence. However, it is clear that the tubule occlusion toothpastes often provide instant improvements for patients with DHS. When used continuously, the benefits of these products may be long lasting.
There are also some curious matters that deserve mention and have presumably arisen because of the role of marketing within the industry.
There are eight different Sensodyne products with the active ingredient 5% potassium nitrate and one with 3.75% potassium chloride as the active ingredient.
In the USA, Colgate Sensitive Pro-Relief toothpaste is advertised as using ‘Potassium nitrate technology, gets to the nerve faster’ and yet the UK version of the same toothpaste uses Colgate's new and widely promoted ‘Pro-Argin technology’.23
The UK version of Colgate Sensitive Pro-Relief is available in three forms:
Even a dental professional may struggle to explain scientifically how the same calcium carbonate ingredient will have three actions worthy of three different products.
Personal communications between the authors and two of the leading toothpaste manufacturers, GSK and Colgate Palmolive, confirm this.24,25 The wide product ranges are principally driven by consumer feedback, such as the desire for different flavours and a whitening effect. However, no explanation was received for the continued use of products clinically proven to be less effective than others or for the number of products being marketed with the same active ingredients.
Professionally applied products
In addition to toothpastes, there are now numerous products and methods available that dental clinicians can use to manage their patients' DHS. Ideally, such methods should have the following properties:
In general, these products are either a fluoride varnish, such as Colgate Duraphat, that forms calcium fluoride globules to occlude tubules, or clear resins, such as Seal and Protect from Dentsply, and Gluma from Heraeus Kulzer. Dentine bonding agents, when topically applied to the cervical margin of sensitive teeth, are an effective way of reducing DHS.26
Colgate Palmolive produces a prophylaxis paste using the ‘Pro-Argin technology’ and GSK produces a Sensodyne prophylaxis paste using the ‘Novamin technology’.
Sylc, by OSspray, uses a dry powder of calcium sodium phosphosilicate (‘Novamin’), applied with compressed air pressure, as a prophylaxis cleaning agent. This combines with water and saliva to form hydroxycarbonate apatite, which occludes the tubules and immediately reduces DHS.27
Glass ionomer and composite resin materials will have been used to restore root surface cavities. In some situations, a dentist may provide a treatment such as endodontics, for a persistently sensitive tooth, or a periodontal plastic surgery procedure, to cover an exposed root surface. Whilst these are unlikely to be the first choice of treatment for DHS, they will probably have the additional benefit of an improvement in, or elimination of, the DHS symptoms.
Irradiation of exposed dentine with a low-output laser leads to an immediate and prolonged reduction in DHS. This is thought to be via anti-inflammatory effects on the pulp28 and increased cellular metabolism promoting production of tertiary dentine by odontoblasts, which leads to tubular obliteration.29
However, laser treatment is unlikely to become a commonplace first line treatment for DHS. It requires expensive equipment and is not suitable for all cases: it appears that the desensitizing effects are optimal in patients aged 25–35, with reduced effects in older age groups. This may be related to age-related changes in the pulp-dentine complex (eg reduced number and size of odontoblasts and reduced tubular patency).
A strategy for managing dentine hypersensitivity
Dental clinicians are taught and develop strategies for managing all aspects of diseases and conditions. For DHS, useful advice and recommendations have previously been provided.30–32
Consider a person who experiences a short, sharp pain when having a cold drink. They are unlikely to do anything about a single occurrence. If this pain becomes a frequent problem, with each cold drink, they may try to find a remedy to resolve it, rather than just avoiding such stimuli. Numerous advertisements on television, the internet and printed media will offer a solution in the form of a toothpaste for sensitive teeth. A visit to the supermarket will offer a similar number of products, all claiming to be the answer to their problem.
If the toothpaste is quickly effective and provides long-lasting relief, the problem is resolved and the person is satisfied. However, without such a positive outcome, the person may attend a dental appointment and ask for professional help. It is important for dentist and patient that an appropriate strategy is used to diagnose and manage the condition.
History
Patients often suggest that they have sensitive teeth but the presenting condition may be different from that which a dental clinician would diagnose as DHS. It is important to exclude other clinical conditions that can cause similar symptoms.
Examination
In addition to the patient's history, a clinical examination will either confirm a diagnosis of DHS or suggest another condition. Methods used to examine for DHS include:
These will all give a short, sharp pain for the duration that each stimulus is applied.
Ice crystals using ethyl chloride on a cotton wool pledget is too strong a stimulus for DHS and are likely to give a positive result with any vital tooth.
Patient education
If a diagnosis of DHS is made, the patient can be informed about any potential causes for this condition, so that appropriate preventive advice can be given. The intention is that the patient can then make the necessary changes to his/her diet and dental hygiene methods. Advice may be given regarding the following:
Treatment
The sensitive teeth can be polished with a desensitizing prophy paste, such as those available from Colgate Palmolive and GSK. These are able to provide an instant improvement in symptoms and can then be followed by regular homecare with an appropriate toothpaste.
Review and further treatment
For the occasions when the preventive and simple treatments have not been effective, a further history and examination should be undertaken, to ensure that the original diagnosis was correct. If so, a sensitive tooth can be coated with one of the resin sealants such as Seal and Protect or Gluma. Alternatively, other methods can be used in which the dental clinician has confidence.
Conclusion
The problem of DHS will continue and is likely to increase as people keep more teeth for longer and dietary erosion becomes more prevalent. Fortunately, owing to the considerable efforts of dental research groups and dental industries, clinicians and patients now have a selection of products and methods to overcome the condition.
