Article
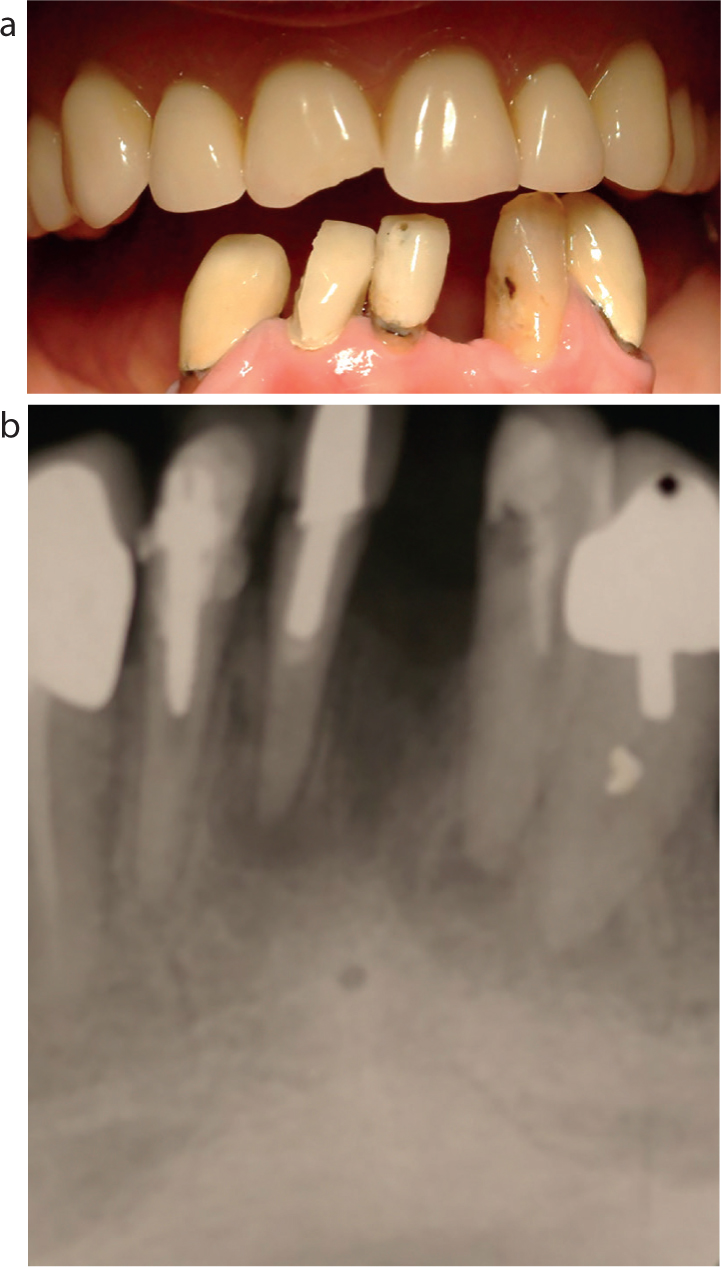
This report describes the treatment of an elderly lady who was referred to me in 2006 because she was unable to cope with a lower acrylic partial denture which she had been advised was necessary following the loss of a lower incisor tooth. She reported that her dentition had been functioning satisfactorily for 40 years without any lower back teeth, adding that she was aggrieved at paying for a denture which she felt wasn't necessary and she couldn't wear. Clinical examination (Figure 1) showed that the patient's current full upper acrylic denture was ill-fitting and damaged while clinical and radiological examination (Figures 2a and b) indicated that the remaining lower incisors had a poor prognosis.

The patient repeated that she didn't want to wear a lower denture but she wasn't in a financial position to consider dental implants.
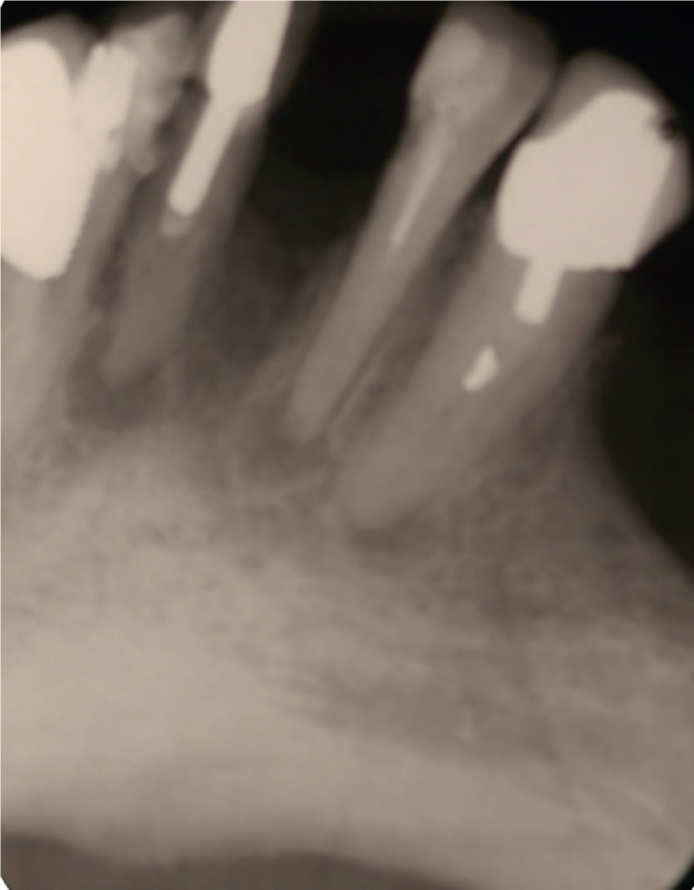
A diagnosis of chronic apical periodontitis of LR21 and LL23 was made: the patient was advised that these teeth had a very poor prognosis. LR12 and LL3 had been restored with post crowns, but the provider had forgotten to root fill the teeth first. Impressions were taken for study models and then, subsequent to a jaw registration, the study models were articulated.
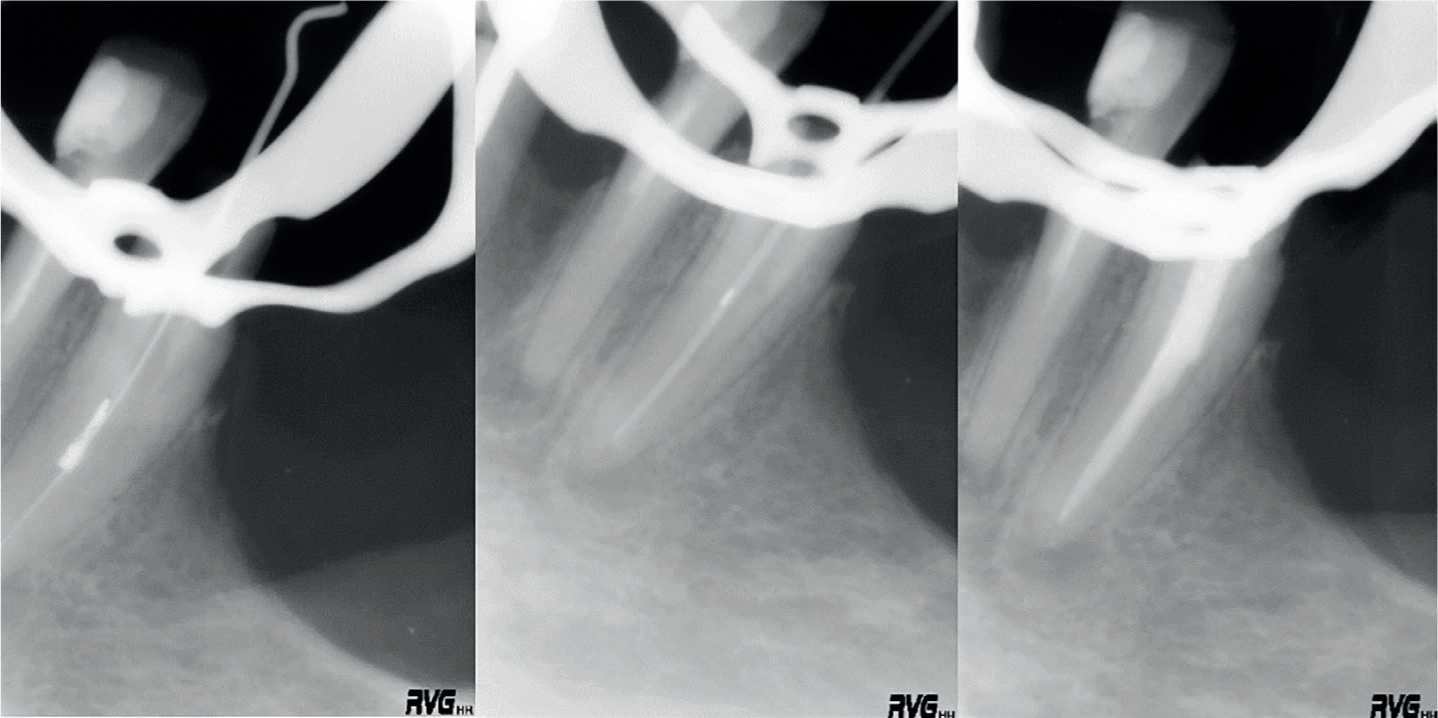
The patient was edentulous in the maxilla and it was considered that, if a fixed bridge could be provided from LL3 to LR3, the forces placed on this bridge would be significantly less than had the antagonists to the bridge been natural teeth. The LL3 potential abutment was restored with a post crown, and no root filling, although there appeared to be a foreign body in the root canal space (Figure 3). It was considered that, if this crown could be removed and the foreign body removed from the root canal, and the tooth receive a root filling, then this tooth would have a reasonable prognosis. Consideration was given to the other potential abutment, the LR3, which was restored with a crown and had previously received what was considered to be an adequate root filling with no apparent apical pathology.
A provisional treatment plan was therefore formulated, but this was dependent upon successful root canal treatment of the LL3.
Root canal treatment was successfully completed (Figure 4) and, further to discussion with the patient, plans were made to provide a fixed bridge from LL3 to LR3 to replace the three remaining and one missing lower incisor teeth.
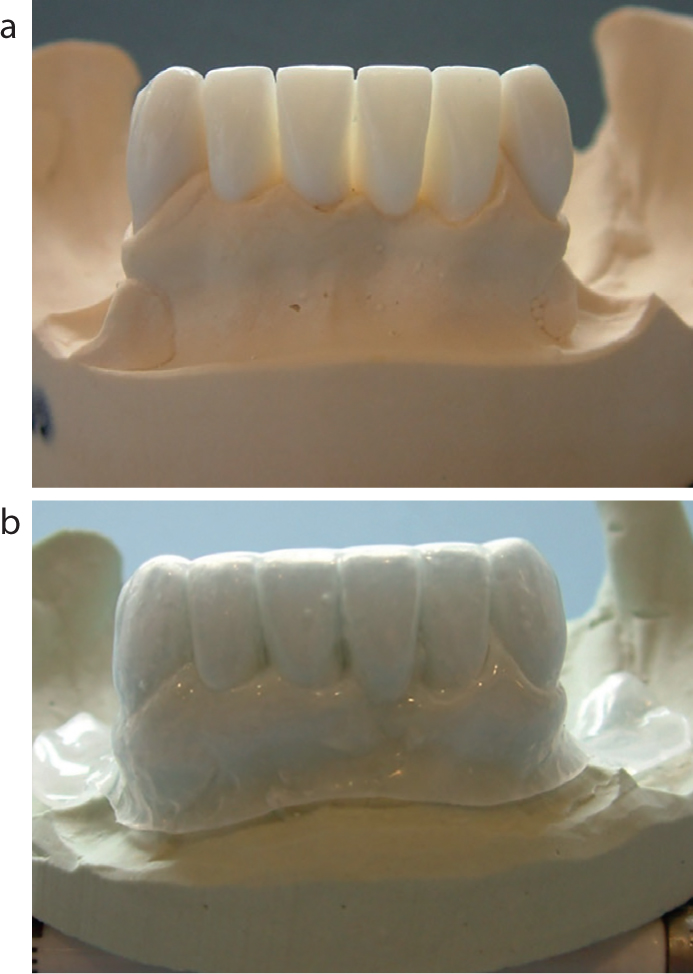
Diagnostic wax-ups were undertaken and a vacuum-formed matrix was made (Figure 5). Subsequent to the root canal treatment of the lower left canine, both lower canines received fibre posts and composite cores followed by temporary resin-based temporary crowns. The lower incisors were removed and a temporary bridge was made, retained by the lower canines.
Following a period of healing, in this case 5 months, the definitive bridge was made. During this time a new full upper denture was completed. Time in practice has taught me to be pragmatic and the one thing I have always been acutely aware of is that we need to contemplate failure when treatment planning. In this case I was concerned that, should I make the bridge at LL3 to LR3 of conventional fixed-fixed design, should it debond on one retainer and remain functional and go unnoticed, a retainer and de facto the bridge could be lost, which would leave the patient with no option but a removable one, the one thing she was most concerned about.
The decision was therefore taken to make two gold copings/telescopic crowns for the canines and the bridge would then be cemented onto these with a temporary cement. In this case, I hoped it was my ‘get out of jail’ card. Should the bridge debond on one retainer, the likelihood would be that the bridge would become loose and fall off (Figure 6).

In the event of any leakage of the temporary cement, the copings, which were cemented adhesively to the underlying fibre posts and cores with Panavia 21 (Kuraray), might go some way to preventing carious destruction of the retaining teeth.
A porcelain fused to metal bridge was made with two additional units cantilevered from the canines to give two additional functioning units. Pink porcelain was used where there had been significant alveolar resorption (Figure 7).

The bridge was cemented with Temp-Bond™ (Kerr) and functioned satisfactorily for 6 years without a debond. Unfortunately, thereafter my patient's health deteriorated significantly and she was unable to attend for any further appointments. She had, however, in the meantime, been able to eat comfortably and socialize confidently without recourse to a removable lower prosthesis (Figure 8).

In this case I considered that the gold copings were instrumental in helping this lady, but we will never know if a conventional bridge cemented directly to the post retained cores in the lower 3s would have functioned equally well.
