Article
Periodontal disease is a chronic inflammatory condition that leads ultimately to tooth loss, masticatory dysfunction and reduced quality of life.1 The 2009 Adult Dental Health Survey (ADHS 2009) highlighted that 94% of the population in England, Wales and Northern Ireland was dentate, meaning that people had at least one tooth.2 Only 17% were considered to have very healthy periodontal tissues and 10% were found to have excellent oral health.2 Of those surveyed, 45% had periodontal disease, with the majority of individuals suffering from mild levels of disease (pocketing between 4 and 6 mm), while 66% had visible plaque on at least one tooth, with 68% exhibiting calculus deposits.2 ADHS 2009 highlighted that 75% of the adults surveyed reported cleaning at least twice daily.2 Globally, in 2015, the prevalence of severe periodontitis was estimated as 7.4%.3 Recently, the burden of periodontal disease was discussed in Dental Update.4
The principles for preventing periodontal disease
The principles for preventing periodontal disease was the subject of the 11th European Workshop on Periodontology on effective prevention of periodontal and peri-implant diseases.5 This workshop aimed to review critical scientific evidence and develop recommendations to improve: plaque control; risk factor control; and the delivery of preventive professional interventions. In terms of preventing periodontitis, it was suggested gingivitis and periodontitis be approached as being one continuum of a chronic inflammatory condition.5 The workshop emphasized regular disruption and periodic removal of accumulating bacterial deposits at, and below, the gingival margin.5 Preventing periodontitis may be primary or secondary. Primary prevention should aim to prevent the inflammatory response from destroying the periodontal attachment by treating the gingivitis through biofilm disruption. Secondary prevention aims to prevent the recurrence of gingival inflammation. Periodontitis can, therefore, be prevented by treating gingivitis and ultimately involves improving patient compliance with patient-performed control of dental biofilms. as well as the provision of professional interventions.
Oral hygiene advice
Oral hygiene advice often includes tooth brushing instructions and information on the use of interdental aids, such as dental floss and brushes. However, one technique of which the reader maybe unaware involves subgingival root brushing. This technique was investigated by Page and Rams in 2013.6 Eleven systemically healthy non-smokers with untreated generalized moderate to advanced chronic periodontitis (old classification) were included in the study, which had a split mouth design and duration of 14 days. The authors investigated clinical parameters, such as plaque and bleeding indices, as well as periodontal pocket depths. They also recorded microbial counts focusing on six putative periodontal pathogens. Each patient had two test sites involving contralateral teeth exhibiting bleeding on probing and pockets ≥6 mm. Baseline measurements were taken, and each side was randomly assorted into a test group (subgingival cleaning) or control (normal brushing regimen). The test subjects completed the subgingival root brushing daily for 14 days after which the clinical and microbial parameters were reviewed and all patients received comprehensive periodontal therapy. The authors reported statistically significant reductions from baseline in the mean plaque and gingival bleeding indices in the test group, as well as with the pocket depths and total subgingival cultivatable counts.6 The test group demonstrated a mean 1.8-mm reduction in probing depths, with reductions in plaque and bleeding on probing indices to almost negligible levels.6 While investigating the subgingival proportions of the six periodontal pathogens, it was found that the test group proportions reduced from 14.1% at baseline to 0.8% on day 14.6 The subjects in the control group who received the normal oral hygiene regimen showed no changes in clinical parameters and furthermore, minimal or no changes in the proportions of the periodontal pathogens.6 The mean 1.8-mm reduction in pocket depths and the microbiological changes in test sites recorded were similar to the changes reported by professional subgingival scaling and root planning.6
Subgingival root brushing can be completed with a variety of brushes, including a single tufted brush or TePe Universal brushes, using a vertical movement down the pocket (Figures 1 and 2).


Case report
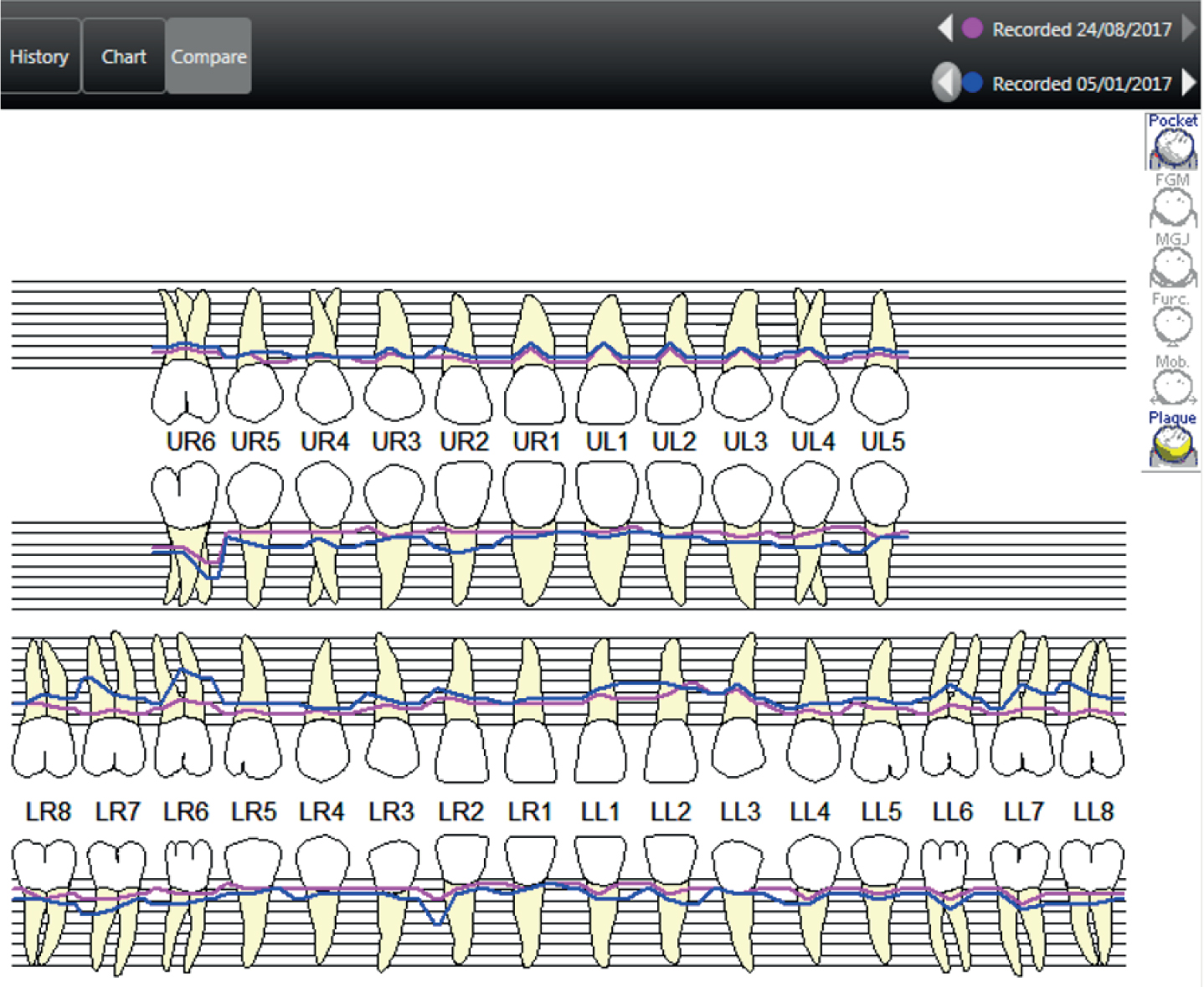
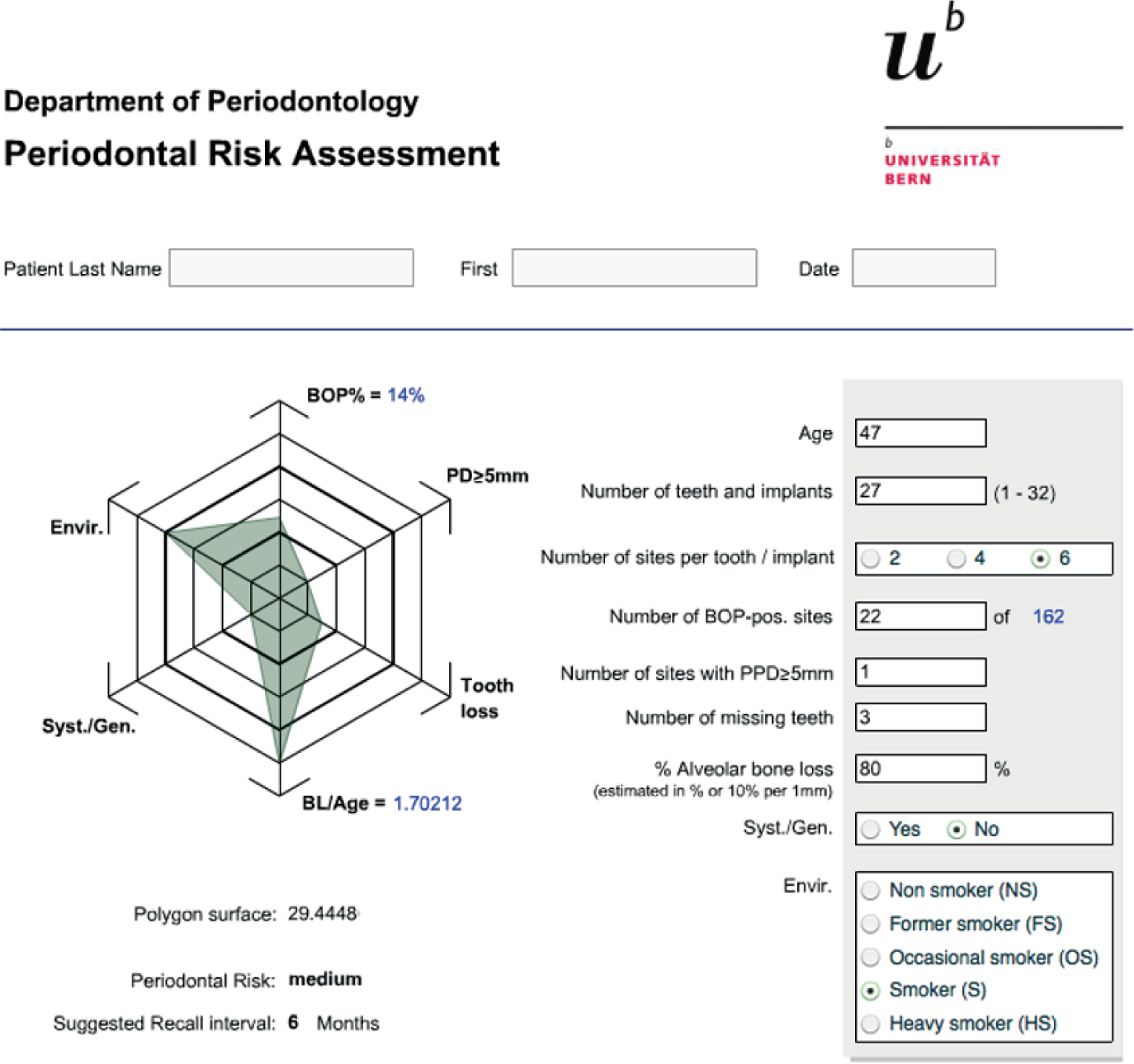
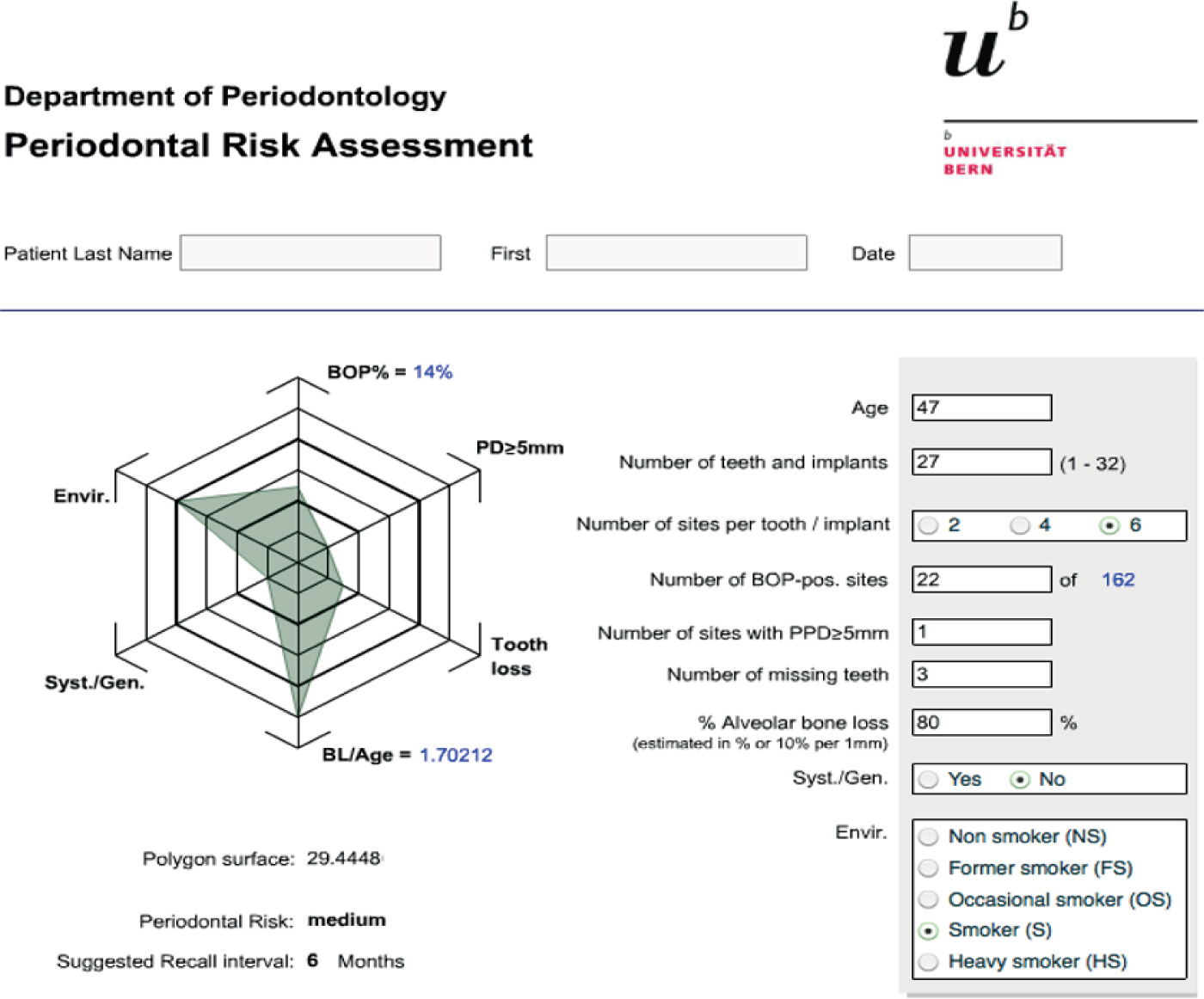
The following case, completed 2017, involved a 47-year-old, medically fit and well male patient who smoked cigarettes and drank alcohol. He also had a family history of diabetes mellitus. His basic periodontal examination (BPE) was 4*34*/4*34* and full mouth peri-apical radiographs and detailed pocket charting (DPC) were completed. A diagnosis (based on the old classification) of moderate to severe, generalized chronic periodontitis was made. Treatment involved tailored oral hygiene instructions, including tooth brushing and interdental cleaning instructions, as well as subgingival root brushing instructions (Figures 1 and 2). The patient was advised to complete subgingival root brushing in the UR6, LR762 and LL8 regions. He also received two rounds of full mouth ultrasonic debridement approximately 3 months apart. A comparison of baseline and post-treatment DPCs is shown in Figure 3. The treatment led to a reduction in the periodontal risk status of the patient as seen by the periodontal risk assessment tool comparison (Figures 4 and 5).7
This clinical case highlights the importance of demonstrating subgingival root brushing to patients with periodontal disease as part of their tailored oral hygiene instructions and treatment care pathway.
