Article
Assessment
A thorough clinical and radiographic assessment of a posterior tooth is essential prior to embarking on endodontic treatment. This is especially important when the tooth is restored with a large restoration, which is commonly the case. It is important that the restorability of the tooth is assessed. Assessment of the amount and quality of remaining tooth tissue from both direct examination and tactile feedback may be of limited value. Deep recurrent disease will often mean that a posterior tooth is not predictably restorable post endodontic treatment, without crown lengthening.
It is essential that every patient is made fully aware of the long-term challenges facing the restoration of broken down posterior teeth, which require endodontic treatment. This allows them to choose and consent to treatment in a fully informed manner. It also allows a comparative discussion with the dentist of other potential treatment options, including extraction and prosthetic replacement, ie with an implant. Part of this discussion might also involve the comparison of fees and the long term value for money of each option.
A bitewing radiograph
It has been frequently reported that an optimally root-treated tooth without a good coronal seal has a greater risk of failure.1 For most endodontically treated posterior teeth, this should be in the form of an indirect cuspal coverage restoration.2 Deep proximal margins, however, mean that it may be difficult to prepare, record a good impression, and cement an indirect cuspal coverage restoration predictably.
Thus it is imperative to assess the quality and quantity of remaining natural tooth structure pre-operatively accurately; particularly the depth and location of the proximal box(es) to the alveolar bone height. A periapical radiograph is the most commonly used pre-operative image used to assess posterior teeth prior to endodontic treatment. This often suffices for anterior teeth (particularly if a small film is used). There is an erroneous assumption that a long cone periapical radiograph (LCPA) provides a parallel image of the tooth. This is rarely the case for posterior teeth because of anatomical restrictions. The floor of the mouth and the palate mean that, for the majority of patients, the image, whilst perpendicular to the beam, is not parallel to the tooth. This has the effect of distorting the anatomy of the tooth and supporting structures, especially in the maxilla, which is less forgiving than the lingual sulcus (Figures 1 and 2).

Figures 1 shows there is little healthy tooth structure remaining on the distal aspect of the UL4, and a poorly adapted restoration on the mesial aspect of the UL6 appears to be encroaching on the biologic width. Using this radiograph alone, the authors would envisage that both teeth would be difficult to restore. However, Figure 3 demonstrates a very different picture from Figure 1. This is due to the limited lingual/palatal overlap of a bitewing, allowing a parallel image perpendicular to the UL4 to be recorded. This allows a more representative image to be recorded of the crown of the UL6 and thus a more accurate pre-treatment assessment of the amount of remaining tooth tissue above the alveolar crest level.
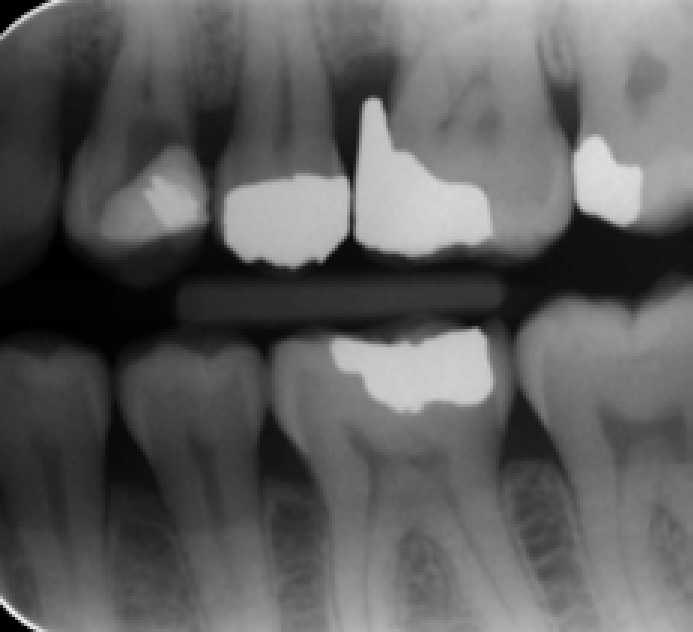
In Figure 3, note that there now appears to be sufficient tooth structure remaining on the proximal aspects of both the UL4 and UL6, which should allow predictable restorations to be placed. In addition, there is an open contact visible between the restorations of the UL5 and UL6. Finally, the access cavity for the UL4 appears to be too large in a mesio-distal dimension, with a thin distal wall of tooth remaining and failure to unroof the pulp chamber. The endodontist should diligently avoid removal of more distal tooth tissue but rather should focus on deepening the centre of the access cavity by 1 mm.
Figure 2 demonstrates the usual angulation of a paralleling device and X-ray tube when taking a lower cone periapical radiograph in the upper right quadrant. Figure 4 demonstrates a more parallel angle allowable with a bitewing view of the same area, for the reasons discussed above.

It is also acknowledged that it may be difficult to achieve a true paralleling technique, because it relies on achieving:
Therefore, there can always be a risk of deviation from the ideal technique, which can result in elongation or foreshortening of the roots. This is one of the major drawbacks of two-dimensional images.
When such an image is used to help assess the status of a heavily restored posterior tooth, it is likely to have the following associated limitations:
For these reasons, the authors recommend that a bitewing radiograph is taken in addition to a long cone periapical radiograph as it is a useful adjunct when paralleling periapical radiography proves difficult. This provides for a perpendicular image of the crown of the tooth and thus a more accurate assessment of the tooth prior to endodontic treatment.
