Article


Patients with cancer may be liable to either osteoradionecrosis or osteochemonecrosis.
Osteoradionecrosis
Radiotherapy (RT) in high doses involving the oral cavity, maxilla, mandible and salivary glands may result in several undesired reactions, of which osteoradionecrosis (ORN) is probably the worst. ORN is defined as exposed irradiated bone tissue that fails to heal over a period of 3 months without a residual or recurrent tumour.
The pathogenesis of ORN is not completely understood but it appears in hypoxic, hypovascular and hypocellular tissue, where there is tissue breakdown leading to a non-healing wound. There is no infection, but teeth in the field of irradiation might be the portal of entry for micro-organisms. ORN, as a radiation-induced fibro-atrophic mechanism, involves free radical formation, endothelial dysfunction, inflammation, microvascular thrombosis, fibrosis and remodelling, and finally bone and tissue necrosis.
Risk factors
Risk factors for ORN include:
Prevention of ORN
ORN is three times higher in dentate than in edentulous patients, which has led to a strategy of preventive extractions of all decayed and periodontally compromised teeth before jaw RT. However, since caries and periodontal disease are so common, there is controversy regarding whether such teeth should always be removed. Patients about to be treated with RT do need intensive preventive dental treatment but it is now generally accepted that teeth that really need to be extracted before RT are only those within the high-dose field that are unrestorable or have advanced periodontal involvement. The extractions must be done before RT, and patients who required multiple dental extractions or extensive surgical extractions, or both, can be given eight weeks of pentoxifylline 400 mg twice daily with tocopherol 1000 IU, starting a week before the procedure, as prophylaxis.
Management of ORN
Hyperbaric oxygen (HBO) has been advocated for pre-operative and post-operative treatment of ORN in high-risk patients having teeth extracted or other operations. A random, placebo-controlled, double-blind study failed to show benefits of HBO over placebo in recovery, in slowing ORN progression, or in relieving pain. Conservative management is preferred, not least since most patients have undergone major surgery before ORN arises and, as a consequence, usually wish to avoid additional jaw surgery, and up to 60% of early and localized cases of ORN resolve with medication and wound care alone. Pentoxifylline (PTX), an antioxidant methylxanthine derivative with an anti-tumour necrosis factor α effect, administered for 6 months, or a combination of PTX and alpha tocopherol (vitamin E), another antioxidant, significantly accelerates healing. The development of myocutaneous flaps and microvascular free bone flaps allows for restoration of mandibular continuity and also brings non-irradiated soft tissue coverage with intact blood supply.
Other innovations are shown in Table 1.
| Innovation | Comments | |
|---|---|---|
| Physical | Ultrasound |
|
| Chemical | Alpha tocopherol (vitamin E) |
Protects cell membrane against peroxidation |
Osteochemonecrosis
Bisphosphonates (BP) are intravenously used (IV-BPs) for treatment of hypercalcaemia of malignancy, as well as prevention of skeletal-related events (SREs) and reduction of bone pain in cancer patients with osteolytic lesions. They are most commonly used in patients with multiple myeloma, breast, prostate, and lung cancers. Oral BPs are used mainly for prophylaxis of osteoporosis, and so are widely prescribed.
Bisphosphonates may cause osteochemonecrosis of the jaw (bisphosphonate-related osteonecrosis of the jaw, or BRONJ) – defined as exposed necrotic bone appearing in the jaws of patients treated by BPs never irradiated in the head and neck area and that has persisted for more than 8 weeks. Most cases (90% +) of BRONJ have been in patients with cancer who received IV-BPs, the cumulative incidence ranging from 1 in 10 to 1 in 1000 but the risk from oral BPs is far lower – less than 1 in 10000.
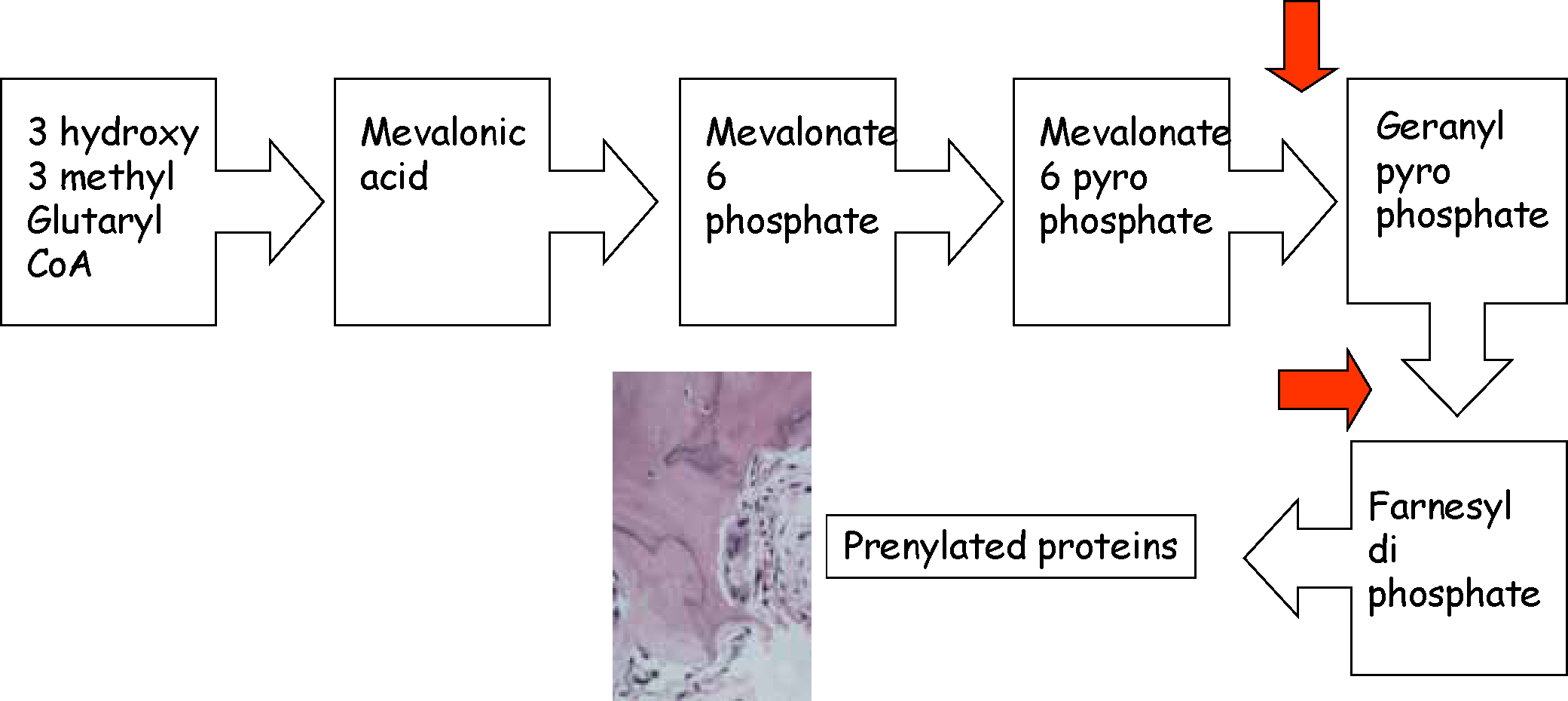
BPs inhibit the HMG-CoA reductase (mevalonate) path, inhibiting osteoclasts, as well as directly inhibiting osteogenesis in bone-healing (Figure 1). In addition, nitrogen-containing BPs induce mucosal cell damage and impede wound healing. The main problem with BPs is the enormously long time they remain in bone and exert these effects – indeed for many years or decades.
Risk factors for BRONJ
Risk factors include systemic and local factors:
Prevention of BRONJ
Prevention is fundamental, since no cure is known. Studies have found an almost three-fold reduction of BRONJ related to zoledronate in myeloma patients after instituting preventive measures (dental screening, all dental work done at least six weeks before starting BPs). One protocol suggested to prevent BRONJ includes the raising of a flap before tooth extraction associated with a broad spectrum antibiotic started three days before, and the flap advanced for primary closure. Results were promising – no cases of BRONJ
Serum collagen telopeptide (CTX) levels, a reliable index of bone turnover rates might predict BRONJ risk but this is controversial. Perhaps CTX monitoring could help determine the best timing for a drug holiday.
Prevention should thus include:
Management of BRONJ
BRONJ diagnosis is mostly from a history of BP therapy and typical clinical symptoms. BRONJ primarily affects the mandibular alveolar bone/mylohyoid ridge area, and features may include:
Lamina dura sclerosis or loss, and periodontal ligament space widening may be early manifestations.
Because BRONJ has a variety of appearances on imaging, the diagnosis cannot be made from imaging alone, though periapical and panoramic radiographs serve for initial screening. CT and MRI provide a more comprehensive evaluation. Bone scans can show abnormal radionuclide uptake 10 to 14 days before bone mineral loss radiographic changes are seen on conventional films. Tetracycline bone fluorescence has recently been used to visualize margins of osteonecrosis more precisely: fluorescence–guided bone resection might improve the surgical therapy of BRONJ. HBO may be a possible adjunctive therapy for BRONJ but has yet to be studied.
Surgical resection generally appears not to benefit patients with BRONJ, so this has led to the restricted use of aggressive surgery in symptomatic patients with advanced BRONJ.
