Glandular Odontogenic Cyst – a Case Report
From Volume 47, Issue 1, January 2020 | Pages 75-77
Article

A glandular odontogenic cyst (GOC) was first introduced as a distinct clinicopathologic entity by Gardener et al in 1988 with the World Health Organization subsequently acknowledging this in 1992. The most common presentation of GOC is a unilocular radiographic lesion2 affecting the anterior mandible of middle-aged individuals with a slight male predilection.3
Presentation in the maxilla is much less common at 30%, compared with 70% of cysts affecting the mandible.2 A GOC can often be misdiagnosed as other cysts of the jaw, including those of a benign or malignant nature,4 due to the non-specific clinical and radiographic features.
Recurrence rates of up to 55% have been reported and occur, on average, 2.9 years following initial treatment.5 Features of GOC which may predispose to higher risk of recurrence are thought to be size, locularity and treatment modality, with higher recurrences seen in large multi-locular cysts treated with enucleation or curettage alone.1 The literature quotes osteotomy or surgical resection as the most suitable option for management of these aggressive cases.6
Case report
A 42-year-old Caucasian male was referred to the Oral and Maxillofacial Surgery Department at Barnet Hospital, London, UK for assessment of ‘a painful recurrent bony cyst affecting the lower right jaw’. The dentist reported that the patient had this lesion treated about 10 years previously, with minimal details available. Medically, the patient had been diagnosed with moderate obstructive sleep apnoea. The patient had no reported paraesthesia and no extra-oral abnormalities. A bony lump was noted in the lower right molar region with buccal expansion.
Radiographic examination revealed a well-defined, well-corticated radiolucency around the region of LR67, unrestored teeth extending to the region of the inferior alveolar nerve (Figures 1 and 2). Further investigations (ultrasound scan and Computed Tomography (CT)) suggested the presence of two separate cystic lesions within the right body of the mandible, with the more anterior lesion positioned inferior to the apices of the roots of the LR6. The second lesion was found to be ramifying between the roots of the LR7 without displacement or erosion of the roots. Expansion of the buccal cortex was noted, and the inferior alveolar canal was preserved (Figure 3).
Subsequently, a list of provisional diagnoses was made:



Following discussion of the possible diagnoses with the patient, options of surgical exploration of the area and biopsy alone, or biopsy and enucleation at the same time, were discussed. Due to the patient's complicated medical condition and lack of sinister appearance, the latter was agreed.
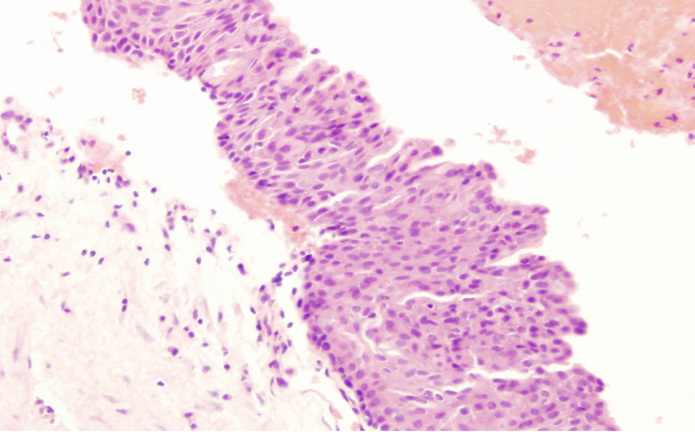
Enucleation of the cyst was carried out uneventfully with two separate cyst cavities identified (buccal and lingual) on surgical exploration. Histopathological assessment reported a multi-loculated cyst lined by non-keratinized, stratified epithelium with scattered mucous/goblet cells and occasional duct-like spaces. The cyst wall in both specimens was fibrotic and showed anastomosing trabeculae of woven bone with no atypia or malignancy noted (Figures 4–6).


The overall report from the clinical, radiographic and histopathological examination indicated a multi-locular GOC affecting the lower right body of the mandible.
The patient was reviewed 6 months post-operatively and he remained asymptomatic. Resolution of the bony expansion was noted (Figure 7). Imaging showed good signs of bony infiltration of the cystic cavities (Figures 8 and 9). The LR6 and LR7 responded to vitality testing throughout the pre- and post-operative period and no further treatment was required, despite the close proximity of the defect to the apices of the abovementioned teeth. The patient will be reviewed again in 6 months.



Discussion
Diagnosis and management of a GOC can be challenging owing to the rarity of the condition and lack of reliable evidence on treatment modalities. This is further complicated by the non-specific clinical and radiographic features of a GOC.
There appears to be no clear guideline on management reported in the literature. Enucleation and curettage has been associated with a higher recurrence rate, however, there is little data available on alternative management strategies, such as osteotomy or surgical resection.
Owing to the risk of recurrence, the literature suggests regular reviews of the patient for up to 3 years, depending on the perceived risk of recurrence.
Conclusion
A GOC is a rare developmental odontogenic cyst which may mimic other cysts of odontogenic origin. Careful clinical, radiographic and histopathological assessment is required for accurate diagnosis. Treatment modalities include enucleation and curettage, as well as osteotomy or marginal resection to treat more aggressive presentations. Post-operative review is recommended due to high recurrence rate. There are some reports of GOC in the literature, however, more clear guidelines on management seem to be lacking.

