References
Hybrid child-friendly biological primary molar restorative alternatives to general anaesthesia
From Volume 45, Issue 8, September 2018 | Pages 728-741
Article

In 2015, and in a Dental Update opening editorial, the management of dental caries under general anaesthesia (GA) in the United Kingdom was labelled ‘a national disgrace’.1 Nearly 70,000 children and teenagers underwent exodontia due to dental caries in the hospital GA environment in the UK between 2013 and 2014, many of which were due to early childhood caries (ECC) with many repeat GAs occurring.1 This has placed emphasis on seeking alternative ways in managing dental caries, especially in young children.
Clinical management of ECC can have a detrimental effect on the long-term health, well-being and quality of life of a child and severe ECC (S-ECC) presents a significant challenge to general dental practitioners (GDPs) and paediatric dentists alike.2 The complexity of the treatment of this disease in early life, resulting from the challenging behaviour management, necessitates the utilization of advanced techniques, most commonly general anaesthesia (GA). The high prevalence of S-ECC caries in our region (UAE)3 in younger age children presents a challenge, however, various models of treatment are offered globally.
Complete oral rehabilitation under general anaesthesia (COR) is a costly procedure, with a witnessed increase in frequency for both healthy and special needs patients,4 with the cost paid by public or private medical insurance.
The paradigm shifts in management of dental caries, including the employment of the biological approach for treatment of dental caries, have changed the way children are treated. Examples for the biological approaches include atraumatic or alternative restorative technique (ART),5 interim therapeutic restorations (ITR),6 indirect pulp capping (IPC)7 and the Hall technique (HT).8
A recent multicentre retrospective evaluation of outcomes of both the biological method of treatment represented by the Hall technique of placement of preformed metal crowns (PMC) and the indirect pulp therapy technique (IPT), and the conventional method of complete caries removal and/or pulpotomies, concluded that both the conventional and biological treatment approaches had similar final outcomes and were equally successful for the management of carious lesions in the primary dentition.9 The combination of both the desire to limit the number of cases treated under general anaesthesia, coupled with the overwhelming evidence in the literature7,8,10 in support for the utilization of the biological approach (Hall technique, IPT) for the treatment of dental caries, led the Paediatric Dentistry Faculty at the Hamdan Bin Mohammed College of Dental Medicine (HBMCDM), Mohammed Bin Rashed University of Medicine and Health Sciences(MBRU) to adopt a unique approach to dealing with S-ECC.
Atraumatic/alternative restorative technique (ART)
The atraumatic/alternative restorative technique (ART) has been endorsed by the World Health Organization as a means of restoring and preventing caries in populations with little access to traditional dental care.5 A recent systematic review concluded that ART restorations have similar survival rates compared to conventional treatment and can be considered an option to restore occluso-proximal cavities in primary molars.11
Interim therapeutic restorations (ITR)
The interim therapeutic restorations (ITRs), as defined by the American Academy of Pediatric Dentistry,6 utilize similar techniques to ART but have different therapeutic goals. ITR more accurately describes the procedure used in contemporary dental practice in the USA. ITR may be used to restore and prevent further decalcification and caries in young patients, unco-operative patients, or patients with special healthcare needs or when traditional cavity preparation and/or placement of traditional dental restorations are not feasible and need to be postponed.6 Additionally, ITR may be used for step-wise excavation in children with multiple open carious lesions prior to definitive restoration of the teeth.12 The ITR procedure involves removal of caries using hand or slow speed rotary instruments with caution so as not to expose the pulp. Leakage of the restoration can be minimized with maximum caries removal from the periphery of the lesion. Following preparation, the tooth is restored with an adhesive restorative material, such as self-setting or resin-modified glass ionomer cement.13
The use of ITR in deep carious lesions as a diagnostic tool for pulpal status was investigated by Coll et al.12 The results of this study indicated that, when GIC was used as an ITR for a period of 1 to ≥ 3 months to assess the pulpal status of asymptomatic molars, the success rate of vital pulp therapy was significantly improved compared to when vital pulp therapy was immediately performed without ITR. The ITR placed in proximal lesions significantly improved the success rate of vital pulp therapy, while ITR placed in non-proximal lesions did not have any significant effect on the success rate. The study also found no difference in the success rate of indirect pulp capping and vital formocresol pulpotomy.12
Sealing dental caries in permanent teeth where the carious lesion is partially removed or completely left has been employed as an accepted therapeutic technique by some, with ten year results,14 and current available evidence supports this approach.15
In permanent teeth, the amount of bacteria detected after conventional complete caries removal was higher than that which remained in sealed caries lesions.16
In a survey conducted to assess the opinion of the dentists in the Gulf Co-operation Council regarding sealing decay in primary and permanent teeth, the majority did not believe in sealing dental caries in both dentitions.17
The Hall technique (HT)
The Hall technique (HT) is a non-surgical/non-invasive method used to restore a carious but asymptomatic and non-septic primary molar in a child using a child-friendly approach. It relies on sealing a non-pulpally involved carious primary molar lesion in situ by using a preformed metal crown (PMC) and glass ionomer cement (GIC).18 The PMC is placed on the affected molar after space is created using orthodontic spacers/separators which are applied for three to five days. No local anaesthesia is utilized and no attempt to remove the carious tissue surgically is made. An online manual detailing the HT issued by the University of Dundee, Scotland, UK is available to download freely.8 The evidence-based platform that rolled out the HT was clearly sound and was supported by randomized controlled trials19 and a Cochrane review.20 Controversial issues, like the effect of the PMC placed using the HT on the occlusion because of the slight initial opening of the bite, was found to resolve spontaneously after a month.21,22 In addition, the HT was found to be more cost-effective than a conventional surgical method of treatment. It is now considered in some circles ‘the golden standard’ for managing the multi-surface, non-pulpally involved carious primary molar.23 According to the recent review written by Welbury, the Hall technique of PMC placement is an ideal restoration for a primary tooth in a young child as it is quick and easy for the child to cope with, doesn't require local anaesthesia and has proven efficacy by means of randomized clinical trials.24
The Hall technique manual recommends crowning primary molars that have no signs of irreversible pulpitis with clear radiographic evidence of a band of normal dentine between the pulp space and the carious lesions.8
Case series report and discussion
In this case series report, the therapeutic methods employed in managing five cases is described. All these cases were treated utilizing the biological techniques reviewed in the introduction section. A common factor between all these patients was the presence of S-ECC in children displaying age appropriate pre-cooperative behaviour. The aim of the treatment was to control active carious lesions to prevent further deterioration under child-friendly age appropriate behaviour management techniques.
When caries was present in anterior teeth, the application of interim therapeutic restorations (ITR) to these teeth was performed using glass ionomer cement.6 No local anaesthetic (LA) was used except the occasional topical benzocaine applied to the gingival tissues prior to the fitting of the PMC with the Hall technique.8 A summary of the demographic and clinical data of these cases is presented in Table 1.
| Case | Age at Start of Treatment | Frankl Behaviour Rating Scale25 at the Start of Treatment | Teeth Treated by ITR Followed by Hall PMC | Teeth Treated by Hall PMC Only Without Stabilization | Period of Follow-Up |
|---|---|---|---|---|---|
| 1 | 4 yrs 5 mths | (+) | ULE, LLE, LRE | URE, ULD, LLD, LRD | 18 months |
| 2 | 3 yrs | (-) | ULD, LRE | URE, ULE, LLE, LLD, LRD | 27 months |
| 3 | 4yrs 6 mths | (-) | URD | URE, ULD, ULE, LLE, LLD, LRD, LRE | 29 months |
| 4 | 2 yrs | (-) | URE, ULE, LLE, LRE | None | 42 months |
| 5 | 2 yrs 4 mths | (--) | _ | URE, URD, ULD, ULE, LLE, LLD, LRD, LRE | 33 months |
Case 1 (Figure 1)
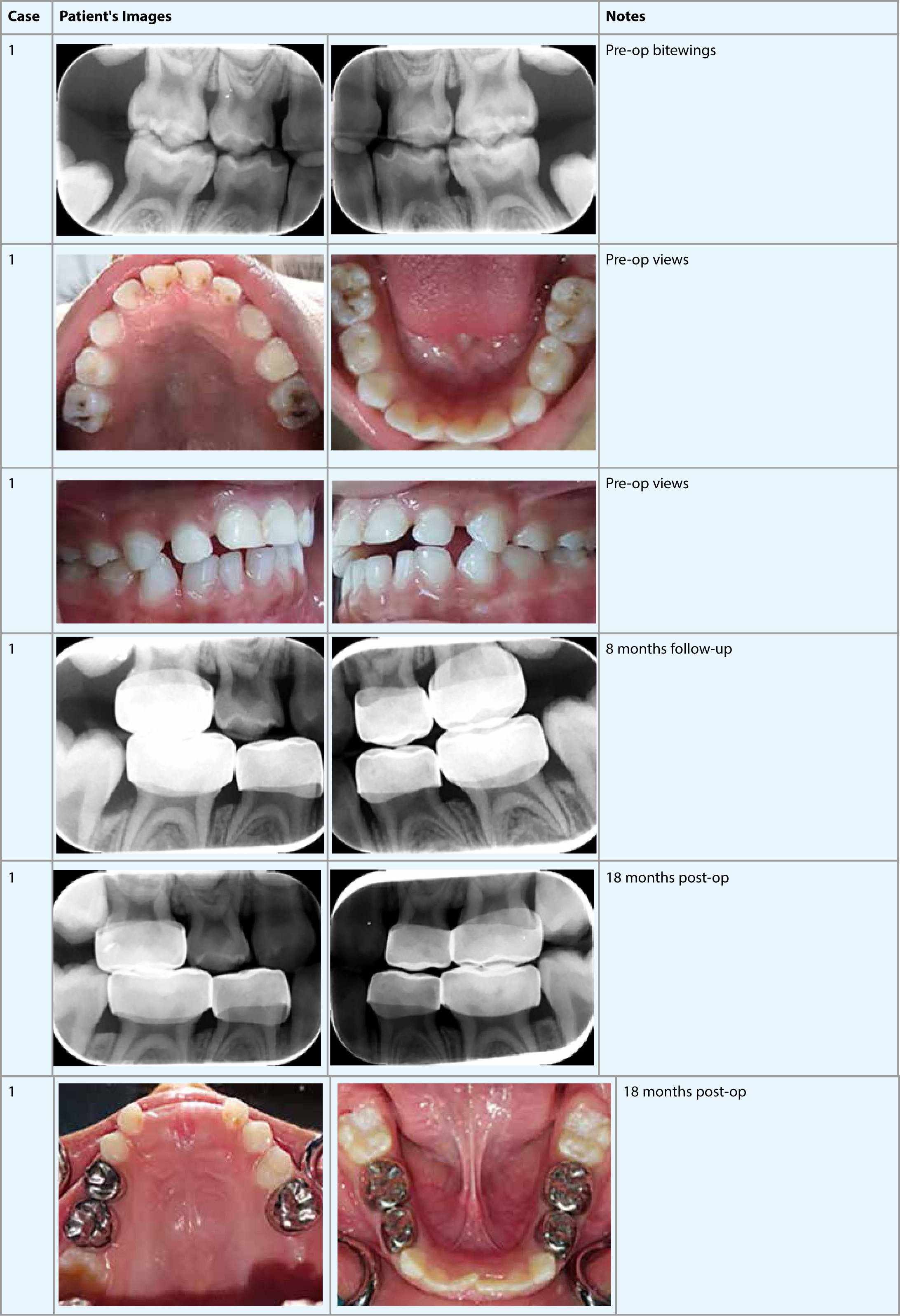
Case 1 describes the treatment of a 4 year 5-month-old boy referred by his GDP for the management of multiple caries under GA. When first seen, the child was pre-cooperative towards dental treatment and his parents were dental phobic. A decision was made to try treatment utilizing biological approaches to avoid the need for GA and to assist the child to become a cooperative dental patient.
ITRs using GIC were performed on ULE, LLE and LRE as they displayed deep open and cavitated clinical caries. The status of the pulp in the aforementioned teeth could not be verified due to inconclusive clinical and radiographic signs and symptoms. To verify the status and confirm the reversible nature of the pulpal inflammation for the deeply carious teeth, an ITR or a ‘stabilization restoration’ was applied.12 The signs of short duration intermittent pain experienced after meals subsided shortly after the placement of the ITRs and did not recur. Following a period of observation ranging from 43 days for LLE, 52 days for ULE and 60 days for LRE, all teeth showed no signs or symptoms of irreversible pulpitis. These primary molars were restored by PMCs utilizing the Hall technique. Coll et al reported significantly higher success rate in vital pulp therapy following a stabilization period of 1 to ≥ 3 months in primary molars.12 The same stabilization idea was adopted but the final restoration of the teeth was substituted from the conventional PMC method with pulpotomy or indirect pulp capping by the Hall technique PMC.
The other primary molars that had radiographic caries were treated with PMC Hall crowns without any period of stabilization following the guidelines of the Hall technique application.8 An enhanced prevention programme was implemented.
The child was regularly followed up for 18 months. All the PMC covered crowns displayed no clinical or radiographic abnormalities. The only non-carious molar (URD) remained caries free. The UR6 is currently under observation for the possibility of ectopic eruption or being caught under the distal PMC of the URE. Lower first permanent molars were sealed shortly after eruption. The child displayed a remarkable improvement in behaviour and acceptance to the dental treatment.
Case 2 (Figure 2)
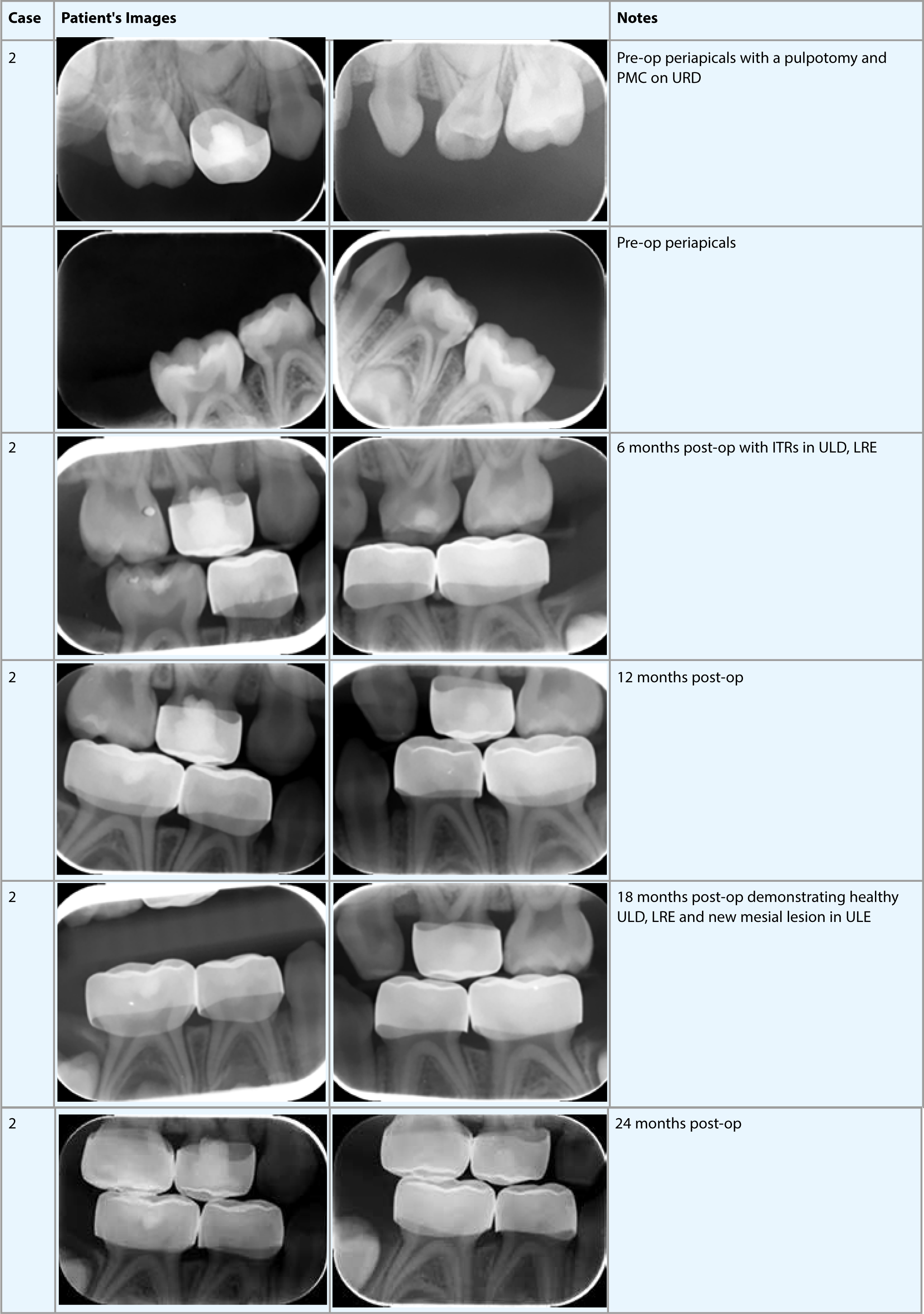
Case 2 describes the management of a pre-cooperative 3-year-old boy treated initially with a pulpotomy and a crown (under LA) on the URD by his GDP which precipitated apprehension towards dental treatment. The child was referred to HBMCDM, and an enhanced prevention programme was implemented. Open cavities with uncertain diagnosis and some history of intermittent pain, as reported by the parents on ULD and LRE, were treated with ITRs or stabilization restorations and left for a period of about 6 months, as demonstrated by the radiographs (Figure 2). It is worthy of mention here that, during the course of treatment, the family travelled abroad for an extended period during the summer holiday, which resulted in the stabilization period for ULD and LRE to be slightly prolonged. Upon the family's return and verification of absence of clinical and radiographic signs and symptoms of irreversible pulpitis, ULD and LRE were restored by PMCs utilizing the Hall technique.
The remaining carious asymptomatic primary molars (LLE, LLD, LRD) were restored using the Hall technique PMC following diagnosis without any waiting period. The 18 month follow-up radiographs demonstrated new mesial caries in ULE and were undiagnostic for URE. The presence of mesial caries in URE was confirmed clinically by placing an elastic separator mesial to the tooth and a PMC Hall technique crown was placed on both URE and ULE. The child was followed up for 2 years. He displayed better age appropriate abilities to cope with dental treatment
Case 3 (Figure 3)
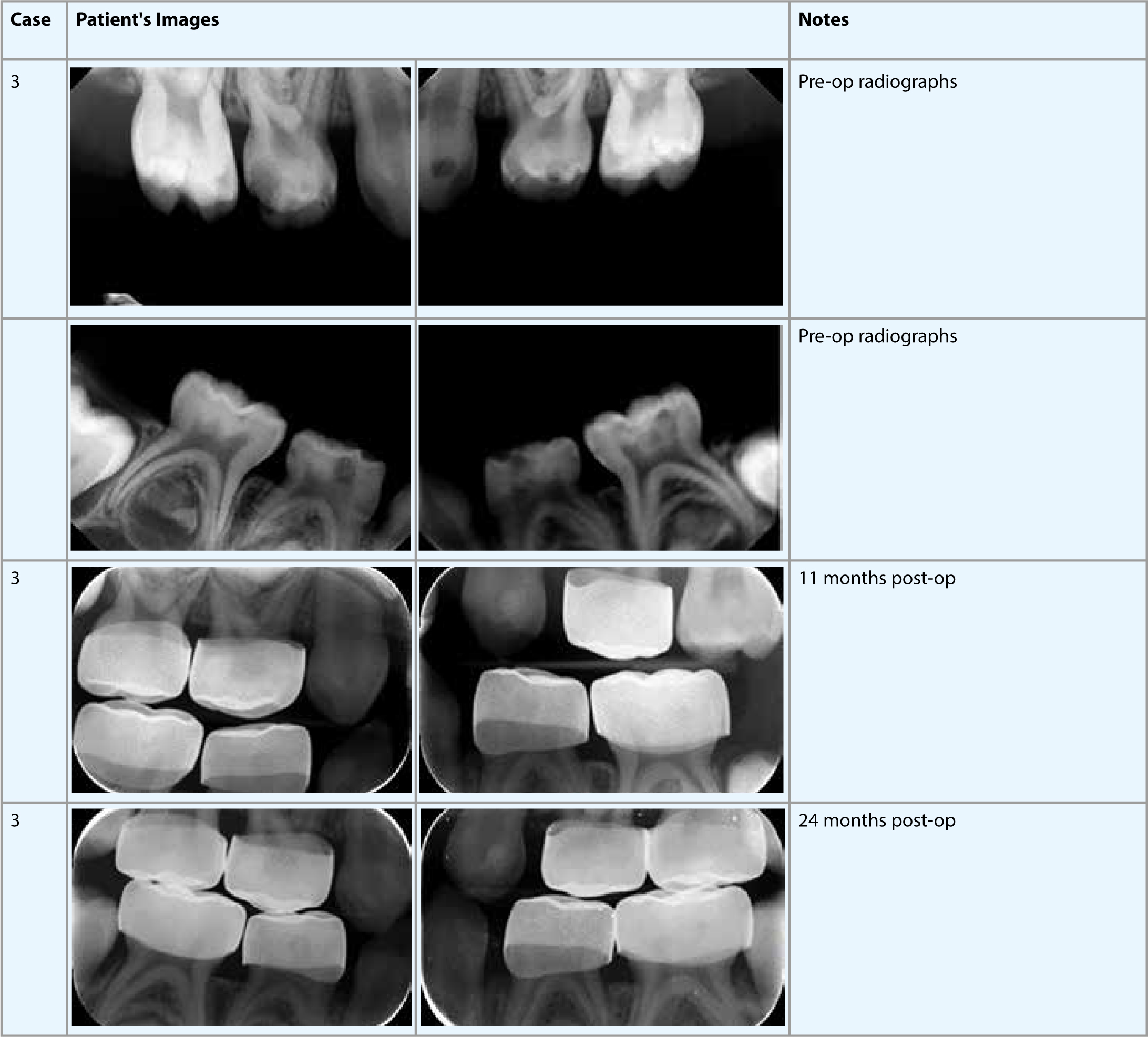
Case 3 demonstrates a similar scenario to Case 2 with stabilization restorations, ‘ITRs’, placed in the URD followed by fitting of a PMC Hall crown on the tooth after about 3 months. The stabilization of interproximal lesions with an interim GIC might pose a challenge for the smooth placement of the Hall technique PMC if care is not taken to contour the ITR properly interproximally. To avoid this problem, care was taken to provide a proper contour to the interproximal surface and the GIC was flossed after the initial setting of the material to allow proper fitting of a rubber separator and a crown when it was appropriate. The separator was placed between points of contact of the molars on natural tooth structure.
PMC Hall crowns were fitted on URE, ULD, LRE, LRD, LLE, LLD without any prior stabilization as they all fitted the criteria for Hall technique PMC placement.8 Tooth ULE was fitted with a PMC Hall crown after 12 months due to the development of occlusal caries.
Case 4 (Figure 4)
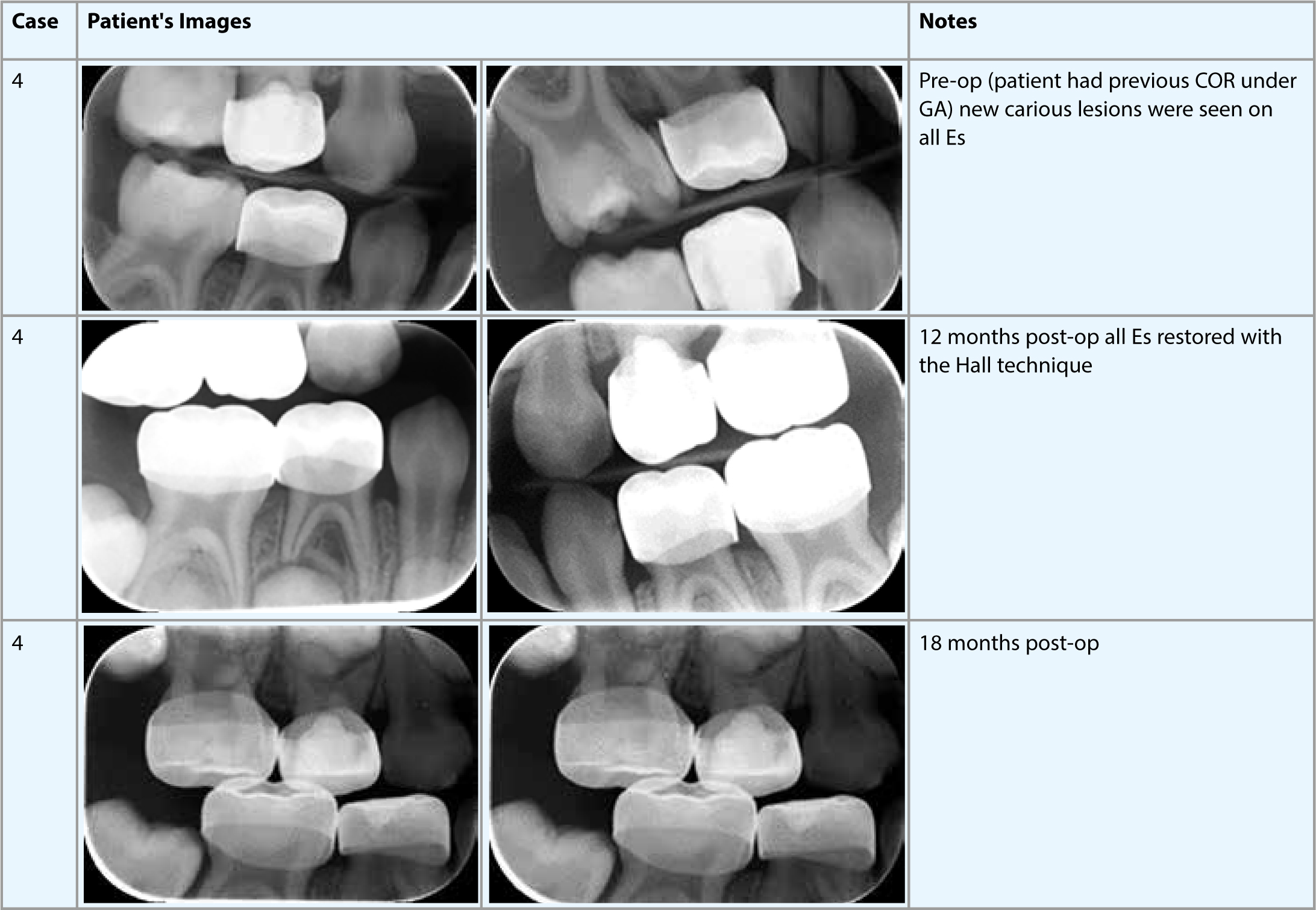
Case 4 is for a girl who was previously treated under general anaesthesia for severe early childhood caries (pulpotomies and PMCs on all Ds and composite restorations of the anterior primary incisors) at the age of 2 prior to the eruption of the second molars. The second primary molars demonstrated enamel defects and caries shortly after their eruption in the oral cavity. Due to the deep nature of the lesions, and to provide proper diagnosis and protection for these teeth but yet avoiding a repeated treatment under GA, all the Es were stabilized with ITRs for a period of about 4 months followed by PMC Hall crowns. As demonstrated by the radiographs in Figure 4, the above mentioned teeth displayed no abnormal signs or symptoms over the period of the follow-up (18 months).
Case 5 (Figure 5)
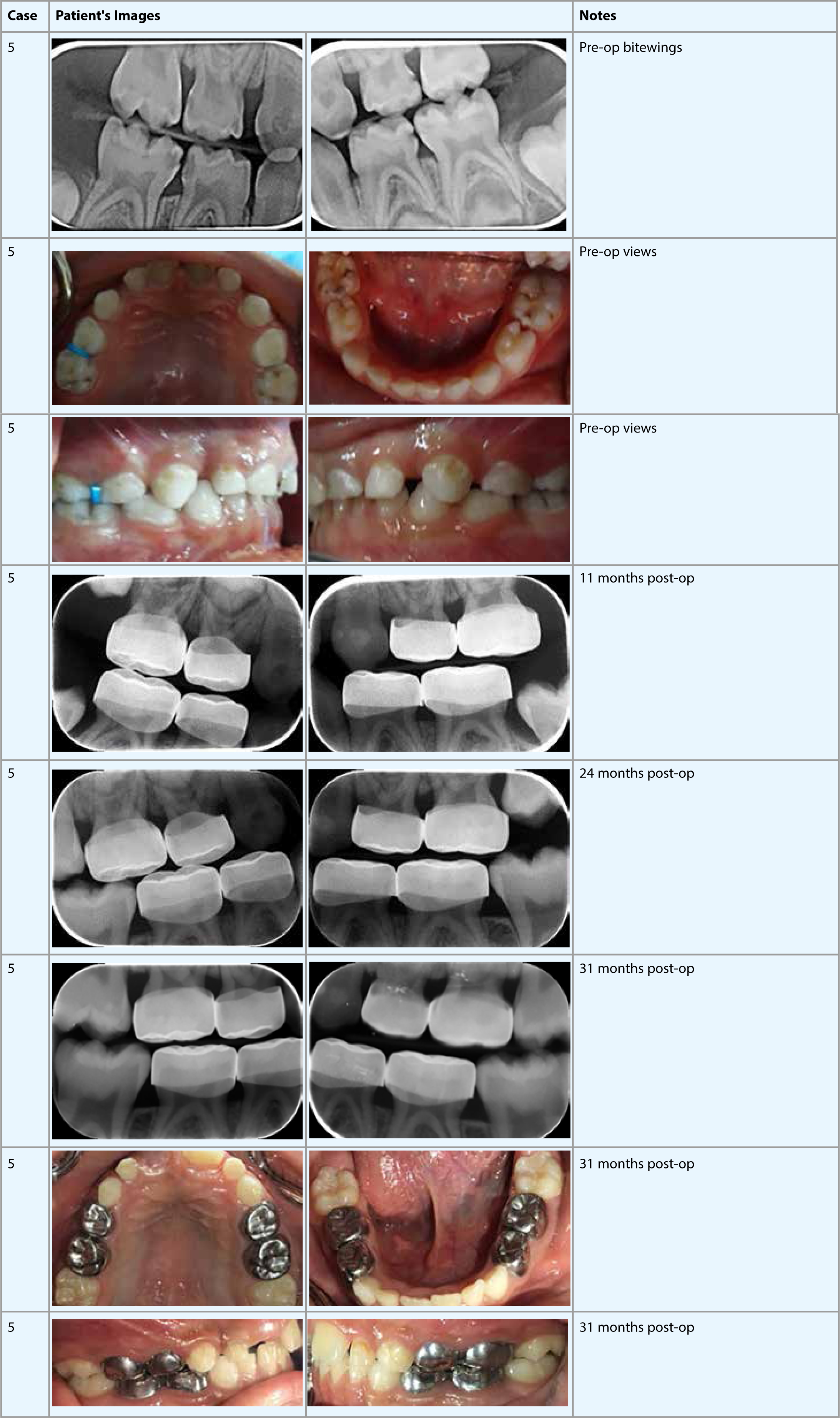
Case 5 demonstrated long term follow-up for an initially pre-cooperative 2-year 4-month-old boy referred to HBMCDM by his GDP for treatment under GA. The child had asymptomatic clinical and radiographic caries and was prescribed an enhanced prevention programme as his parents were keen to avoid GA. He was subsequently treated with PMC Hall crowns fitted on all of his primary molars over a period of two months. He was followed up for over two and a half years. He developed no symptoms and had no radiographic pathology. The only exception was that the crown on the ULE was removed as it prevented the UL6 from eruption, as demonstrated in the 24 month follow-up left bitewing radiograph in Figure 5. A week after the removal of the crown, UL6 erupted normally in the oral cavity and another Hall crown was placed on ULE.
As demonstrated in the reported cases, some teeth with deep carious lesions present a challenge in diagnosis when no specific symptoms or radiographic evidence exists to support a definitive diagnosis. The application of GIC as an ITR for a period of time to confirm the diagnosis of the reversible pulpitis,13 followed by the application of a PMC utilizing the Hall technique, is often utilized in the care of our patients, especially the pre-cooperative ones where the other alternative would be treatment under GA. The use of the PMC Hall technique provided a useful and successful tool in managing children with early childhood caries without the need for any local or general anaesthesia. The technique was also useful in transforming pre-cooperative or potentially cooperative children into cooperative dental patients.
The use of Silver Diamine Fluoride (SDF) has recently gained significant support in scientific paediatric dentistry circles26 but has not been utilized in our cases. This aspect represents an area undergoing renewed interest. A possible combination of the application of SDF followed by PMC Hall crown fitting might demonstrate another useful biological, non-invasive, child-friendly technique.
Conclusion
The reported cases exhibit the utilization of several biological caries management techniques personalized for the individual child. Continuous high quality research is needed for further validation of such methods and for utilization of others. By employing child-friendly methods in both the specialist and the non-specialist GDP environment, where most of the burden of caries in children is managed, a major contribution to the reduction of unnecessary dental GAs for very young children can be made.
