Space Maintenance in the Mixed Dentition – a Necessary Intervention or a Step Too Far?
From Volume 47, Issue 1, January 2020 | Pages 54-60
Article

Management of the paediatric patient presents multiple challenges for the clinician, not just with regard to patient management and compliance, but also in managing a dynamic and changing dentition. Primary teeth serve a purpose to provide aesthetics and function, whilst also maintaining arch length and space for their permanent successors. Premature loss of primary teeth can occur for a number of reasons, such as extractions due to dental caries, trauma, hypomineralization and for orthodontic treatment.1, 2, 3, 4, 5 Unplanned, early loss of primary teeth can result in unwanted migration of permanent teeth into the space, causing loss of arch length, crowding, displacement of teeth and therefore malocclusion. These deleterious effects increase the likelihood of future orthodontic intervention.6 Dental practitioners can take measurable steps to retain space in the mixed dentition to ameliorate potential unwanted effects in the permanent dentition.
Space loss
Premature loss of primary teeth can occur for a number of reasons, such as dental caries, trauma and ectopic eruption of permanent teeth.2,7 The effects on the permanent dentition can potentiate or directly cause a number of deleterious effects, the most common of which are outlined in Table 1.7
| Effects on the permanent dentition |
|---|
|
|
Primary anterior teeth
Primary incisors are prone to premature loss due to increased susceptibility to dental trauma and early childhood caries. Premature loss of a primary incisor does not normally have an impact on space loss. There may be some movement of the erupting permanent incisors into the resulting space, however, this is commonly seen during normal exfoliation and eruption, therefore space maintainers are not commonly used.8
The premature, unilateral loss of a primary canine has been shown to have a significant effect on the centreline and a balancing extraction must be seriously considered as a preventive action.9 This may not, however, be an issue in the spaced dentition, but these patients need careful monitoring with a full explanation of the risks to the parent/guardian. Bilateral, early loss of mandibular primary canines can result in lingual movement of mandibular incisors and therefore loss of anterior arch length. These cases are likely to be due to severe early childhood caries or severe crowding, resulting in premature exfoliation of the mandibular primary canines. Referral for specialist orthodontic management is warranted for assessment and consideration of lingual arch placement.10
Any initial aesthetic concerns caused by primary anterior tooth loss are likely to be about the sudden change in appearance. Parents should be reassured about both future long-term aesthetics and function. Any immediate speech difficulties and alterations usually resolve.8,11
Primary molars
Premature loss of a primary first molar can result in loss of space of approximately 1.5 mm in the mandible and 1 mm in the maxilla. This is, however, likely to be clinically inconsequential for most patients.12 Therefore, the use of a space maintainer is not routinely recommended.13 It is of note that unilateral loss of a primary first molar may occasionally have an effect on the centreline, hence careful monitoring is advised. If extractions under general anaesthesia are planned, consideration could be given to concurrent balancing extractions involving both primary first molars, to minimize risk of future centreline disturbances if this is thought to be a significant potential problem. This will also minimize the interproximal caries risk for the primary second molar and distal surface of the primary canine, which hold an important role in space maintenance. Orthodontic input should be sought for any cases that may require future orthodontic treatment or treatment planning based on a complex presentation.9
The primary second molar plays an important role in preserving leeway space, which is the difference in mesio-distal width of the primary canines and molars compared to their succeeding permanent canines and premolars (2.5 mm per side in mandibular arch and 1.5 mm in maxillary arch). The greatest size discrepancy exists between the primary second molar and second premolar, which is referred to specifically as the ‘E space’.14 This space facilitates mesial movement of the first permanent molar, the effects of which are greater in the maxilla compared to the mandible.15
An actively erupting first permanent molar will migrate mesially if there is a missing primary second molar causing localized loss of space, with resultant crowding and overall loss of arch length.16,17 This loss of space has significant implications for Class II malocclusions, which may as a result require extraction-based orthodontic plans due to mesial drifting of maxillary first permanent molars, or need additional anchorage supplementation with headgear or temporary anchorage devices.16
Space maintainers
Ideally, the best space maintainer is the primary tooth itself and every attempt should be made to retain the tooth as part of the natural dentition. There are numerous methods of restoring carious primary teeth, with the Hall Technique reported as one of the more successful means of managing caries in the primary dentition.18
There are many types of artificial space maintainers and those independent of fixed appliance treatment are discussed. Space maintainers are usually cemented with a quick-setting luting cement, such as glass ionomer cement. Both fixed and removable space maintainers can accumulate plaque and predispose the patient to dental caries, hence careful patient selection is required (Table 2). It is therefore essential to minimize the risk of caries through dietary advice, reinforcement of oral hygiene and application of fluoride varnish in accordance with Delivering Better Oral Health guidelines.19
| Patient selection for space maintainers |
|---|
|
|
Band and loop
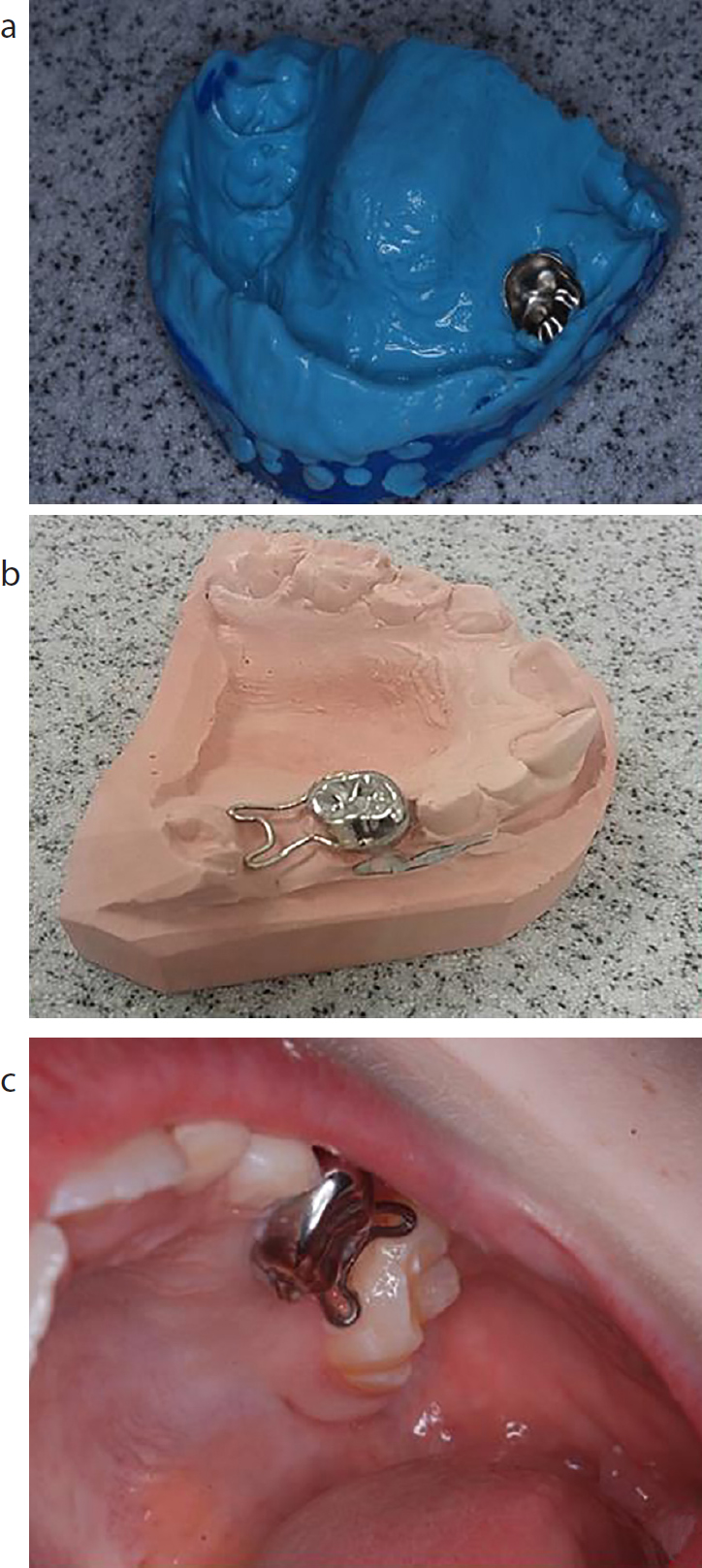
One of the most commonly used space maintainers is the band and loop appliance.20 This involves placement of a pre-fabricated orthodontic band around the first permanent molar and an alginate impression taken with the band in situ. The model is cast with the band in place and orthodontic wire shaped to engage the tooth mesial to the space, which is soldered to the band. The space maintainer can then be cemented in place (Figures 1 and 2) Alternatively, there are pre-fabricated metal and plastic band and loop appliances that only require a single visit.21 Reasons for failure can include breakages at the solder joint or decementation of the band.22


A crown and loop space maintainer is a similar appliance that involves a pre-fabricated stainless steel crown, providing full coverage with a soldered loop overlying the space to be retained (Figure 3). One prospective study reported a significantly higher failure rate for band and loop space maintainers (83%) compared to crown and loop (22%).23
Fibre-reinforced composite
Fibre-reinforced composite (FRC) in paediatric dentistry involves bonding a strip of polyethylene fibre to adjacent teeth and contouring a composite pontic to create an aesthetic space maintainer.
A pre-operative impression is ideally required to produce study models that allow space and occlusal analysis. There should be sufficient clearance for the fibre strips on abutment teeth.24 The FRC space maintainer can be constructed on the model and then bonded intra-orally using composite (Figure 4). This reduces chairside time and reliance on patient co-operation, however, it is possible to create the bridge intra-orally in a single visit. Its use is limited to single posterior deciduous teeth.25 Primary anterior teeth have limited and progressively diminishing clinical crown height and are the first teeth to exfoliate, hence provision of a FRC space maintainer would not be appropriate.

Plaque can stagnate superiorly and inferiorly around the fibre strip and debonding of one side can predispose to caries, hence regular follow-up is required. The younger patient requires careful assessment for plaque control, amenability to dental treatment, including co-operation for impressions and moisture isolation, ideally under rubber dam. Debonding is a common reason for failure at both the enamel-composite and fibre-composite interface. However, one advantage is the ease and possibility of repair with additions of composite.20,26 Involvement of adjacent teeth may compromise their exfoliation or might lead to failure of the space maintainer once the retaining primary teeth become mobile.25
Lingual and palatal arches
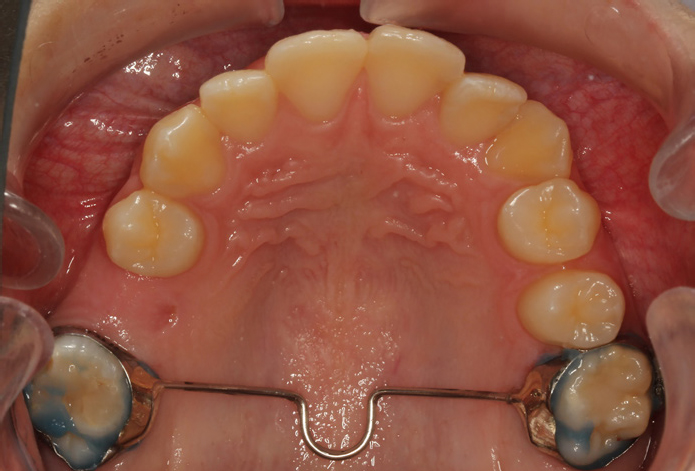
The lingual arch is a space maintainer constructed of round archwire normally attached to the first permanent molar using stainless steel bands (Figures 5 and 6).


They prevent mesial movement of the first permanent molar, therefore preserving arch length.27,28 The lingual arch is useful when there are bilateral posterior teeth missing in the young patient, thus preventing other forms of space maintainers being appropriate. As the appliance is cemented in place, it is likely to be more tolerable and effective than a lower removable appliance. An alginate impression is taken over pre-fabricated molar bands and a working model cast. A lingual arch is formed and soldered into position.29 The archwire engages the lingual enamel of the lower teeth, hence, forward molar drift is prevented.
The mechanism of the transpalatal arch (TPA) is similar to the lingual arch, comprising stainless-steel bands placed on the maxillary molar teeth with a wire spanning the palate (Figure 7). Its main uses are in preventing mesial movement of the molars and preventing spontaneous space loss, thus providing future anchorage for orthodontic treatment. The TPA should be considered in cases of bilateral loss of the maxillary second primary molar when space is at a premium, in an attempt to maintain ‘E’ space.30 This is often of concern in patients with Class II malocclusions where the TPA may mitigate the need for an extraction-based orthodontic treatment plan, or may prevent turning a simple extraction case into a maximum anchorage case. The Nance appliance is similar in design, with bands around the maxillary molars soldered to wire and a large acrylic button in contact with the vertical part of the hard palate.31 Both the TPA and Nance appliance are simple yet effective appliances, however, some disadvantages include soft tissue trauma to the palatal mucosa, particularly when the button is poorly positioned or too small, patient intolerance and occasional fracture of the appliance.32 In addition, the bands around the permanent molar teeth will predispose them to plaque accumulation and patients should be closely monitored due to their increased risk of dental caries.
Distal shoe appliance
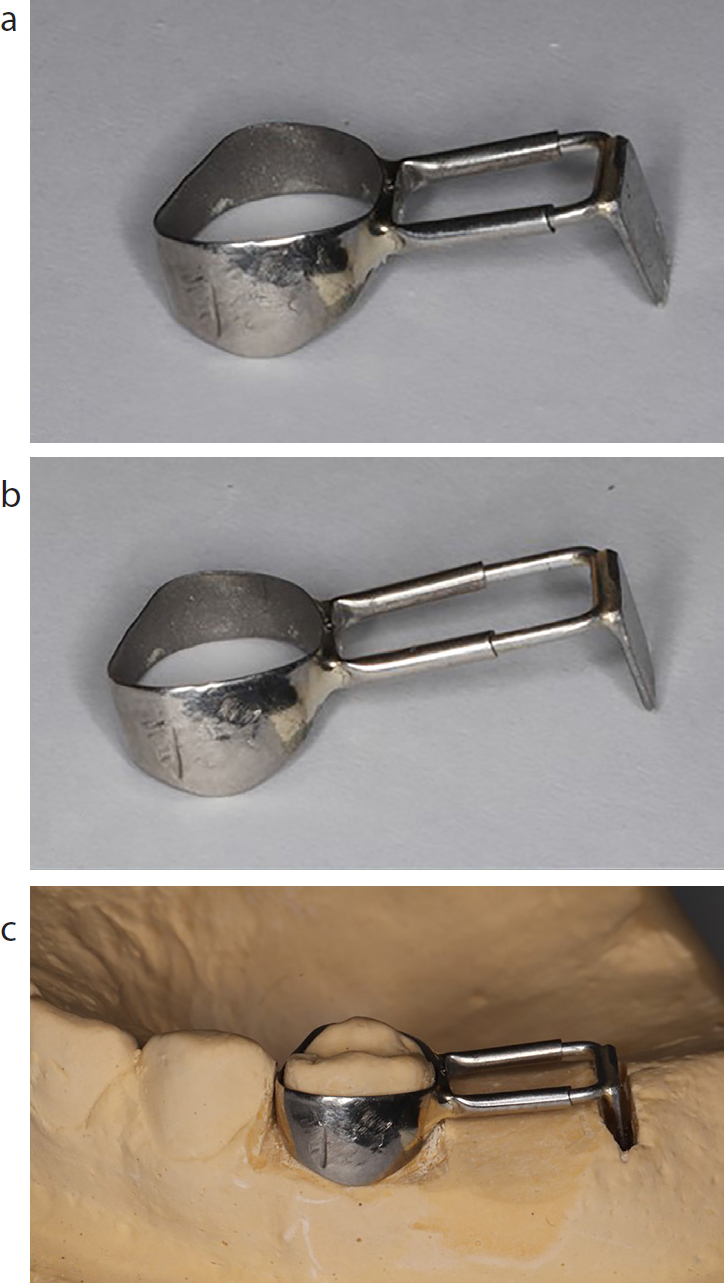
The distal shoe appliance is a variant of the band and loop appliance for space maintenance following the loss of a second primary molar prior to the eruption of the first permanent molar tooth (Figure 8). It involves the placement of a pre-fabricated stainless steel crown or band on the primary first molar, with a distal wire conformed to an adjustable ‘U’ shape and soldered to the crown. The terminal part of the ‘U’ bend can have a metal guide plane that extends subgingivally to contact the first permanent molar and guide its eruption.33 The appliance provides full coverage of the primary first molar, opposing mesial movement of the first permanent molar, with such robust construction reducing the risk of fracture. Once the first permanent molar has sufficiently erupted into position, the appliance can be replaced with a more hygienic design of the traditional band and loop.34 Correct contouring of the terminal part of the ‘U’ bend is essential to prevent damage to the erupting first permanent molar or second premolar.35 This technique is rarely utilized due to the difficulty of correct positioning of the distal shoe and the need to place the appliance under local anaesthetic.
The most common reason for failure of any fixed space maintainers is failure of the soldered joint. Other reasons include decementation, interference with eruption interference with eruption of the permanent dentition and pathological involvement of the abutment tooth.22,36 Nevertheless, fixed space maintainers overcome the requirement for excellent patient co-operation with removable appliances, which were perhaps more commonly used in the past.37 Regular reviews are required to check the integrity of the appliance, ensure that it is functioning as intended regarding maintenance of space, and also for vigilant surveillance and prevention, as the appliance can predispose patients to gingival disease and dental caries.
Conclusion
Implementing a proactive, preventive approach for preserving space is ever more feasible and should be strongly considered in the low caries risk dentition. Significant benefit can be gained for the patient by this early intervention, rather than dealing with the future ramifications of loss of space. Currently, space maintainers are considered orthodontic appliances and can only be provided on the NHS by practices contracted to carry out orthodontic treatment.38 Dental practitioners who do not hold such a contract can refer to specialist orthodontic services.
This review of space maintainers highlights a topic which may not be covered in detail in the undergraduate curriculum and provides topics to be considered for continuing professional development. In addition, this review emphasizes the importance of judicious treatment planning, caries risk assessment and the range of options for space maintenance, which should be considered as part of a holistic approach to care for the young patient.
