Article

Wearing gloves and proper hand hygiene (HH) are two major tenets of today's dental office infection control programme. In fact, the two activities are mutually inclusive. Their protective success depends on the correct application of the other.
Wearing gloves does not eliminate the need for HH. Rather, frequency of HH must increase. HH should be performed immediately before donning gloves. Lowering microbial contamination decreases the chances of soiling the non-sterile glove supply when reaching for new gloves and decreases transient skin flora. Gloves can have small, unapparent defects or be torn during use. Also, hands can become contaminated during glove removal. These circumstances increase the risk of operative wound contamination and exposure of dental healthcare professionals' (DHCPs') hands to patient micro-organisms. In addition, bacteria can multiply rapidly in the moist environments present underneath gloves. Hands should be dried thoroughly before donning gloves and washed again immediately after glove removal.1
Personal protective equipment (PPE) refers to wearable equipment that is designed to protect DHCPs' personal clothing and skin from exposure/contact with infectious agents. Dental PPE includes gloves, face masks, protective eyewear (goggles and face shields) and protective clothing (eg reusable or disposable gowns, jackets and laboratory coats). Gloves are used in situations involving possible contact with patient blood or body fluids, mucous membranes, non-intact practitioner skin (eg exposed skin that is chapped, abraded or has dermatitis) or other potentially infectious materials (OPIMs).1,2
Gloves protect the wearer, the patient currently being treated, other DHCPs, subsequent patients, the immediate environment and even family members. Gloves are universally used in healthcare, involving many direct patient care procedures including surgery, laboratory activities and environmental cleaning. Gloves enhance patient and practitioner safety. It is important to keep the environment as clean as possible so that it does not become a source of microbial transmission.3
Because gloves are task-specific, their selection should be based on the type of procedure to be performed (eg surgery or patient examination). Sterile surgeon gloves are FDA (US Food and Drug Administration) cleared medical devices and are less likely than patient examination gloves to harbour pathogens or have defects that could contaminate an operative wound or practitioner skin. Sterile gloves are reserved for invasive procedures. Non-sterile patient examination gloves are also FDA regulated and are used in patient care, examinations, other non-surgical procedures involving contact with mucous membranes and laboratory procedures.1,2,3
There is no evidence that differences exist concerning safety or clinical effectiveness among differing types of gloves. Also, there are no differences between latex and nitrile gloves concerning touch sensitivity or psychomotor performance. It is always best to know how to use gloves correctly.3
There are several practical admonitions. These include:
Personal protective equipment is donned in a specific sequence − gown, mask, protective eyewear and, finally, gloves. Hands are inserted into the gloves and pulled up and over the gown's cuff, covering all skin surfaces.3
PPE must also be removed in a prescribed sequence. After treatment, most of the patient's body fluids have been deposited on outer PPE surfaces. Care must be taken not to contaminate skin, mucus membranes, underlying clothes and the local environment. Removal should be by level of contamination, with the most soiled coming off first. The removal order is gloves, followed by protective eyewear, gowns and masks.1,3,4,5
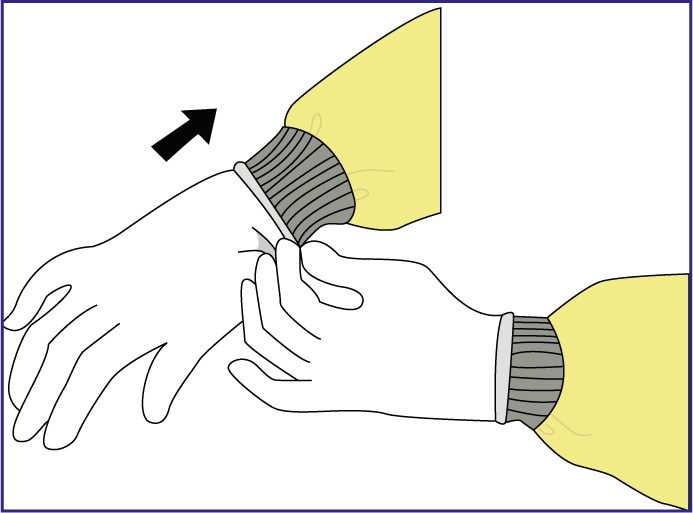
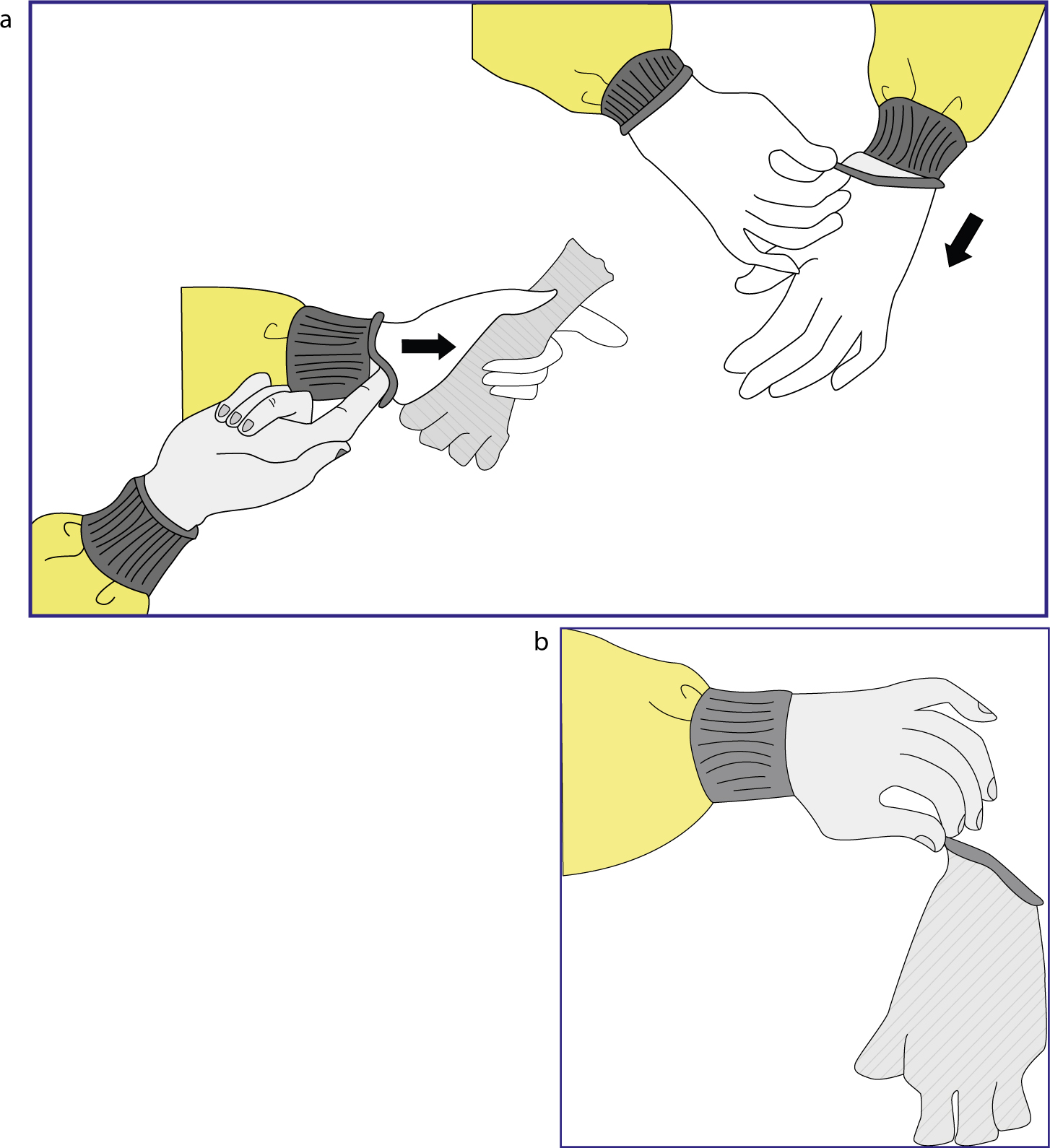
To remove gloves correctly, grasp the outside edge, near the wrist, peel away from the hand, turning the glove inside out. Hold the removed glove in the gloved hand. Then, slide an ungloved finger under the wrist of the remaining glove and peel off from the inside, creating a bag containing both gloves. Discard and perform HH.3,4,5
Hand hygiene is the most important measure to prevent spread of infections among patients and DHCPs. Education and training programmes should thoroughly address indications and techniques for HH practices before performing routine and oral surgical procedures.1,2
HH should be performed when:
For routine dental examinations and non-surgical procedures, use water and plain soap (hand-washing) or antimicrobial soap (hand antisepsis) specific for healthcare settings or use an alcohol-based hand rub (ABHR).2
Soap and water hand-washing generally is not affected by organic materials and should be used when hands are visibly soiled (eg blood, body fluids). Soap and water are effective when properly performed, are familiar to DHCP or produce few allergies. Use can dry the skin and cause irritations, though these can be prevented or treated well with hand lotions. The learning process takes some time and usually requires a sink and running water.2
ABHRs are now broadly available and widely used and have the following qualities:
For surgical procedures, perform a surgical hand scrub before putting on sterile surgeon's gloves. For all types of hand hygiene products, follow the product manufacturer user instructions.1,2,3,5
Traditionally, HH compliance among all healthcare professionals has been suboptimal. Things have improved over the last ten years because of increased awareness, in-service training and increased electronic and visual monitoring. This is essential because there is a direct relationship between proper HH and the rate of healthcare-associated infections among patients and practitioners.1,2,3
When assessing performance, it is important to review possible behavioural aspects that might be affecting compliance. New tools and innovative technologies are constantly emerging; however, whistles and bells cannot replace proper basic HH practices. Stressing the importance of HH and encouraging personal responsibility and collaboration should help improve compliance. Many mistakes are small, but often they add up to become a large problem. Gloves can help reduce the risk but, if used inappropriately, may contribute to the problem.3
